Decision Support on Your Phone: Apps That Promote Better Guideline Adherence
 An Interview with Jeff Dunn, DO, MBA, CEO of Redivus Health
An Interview with Jeff Dunn, DO, MBA, CEO of Redivus Health
Is better decision support/guideline adherence an issue that payers need to tackle and support?
Yes, I think it’s a two-pronged approach. Hospitals and providers need to make sure they are practicing with a focus on quality and patient safety. Payers should also be aligned around that strategy to do what is best for the patient. Payers should also focus on the triple aim of health care. Those three dimensions are improving the patient experience of care (quality and satisfaction), improving health of populations, and reducing the cost of health care. Improving care and lowering cost can be made possible by standardizing best practices via better decision-
support systems.
Can you explain how Redivus works? And how it differs from other decision-support tools?
Redivus Health is unlike current decision-support tools out on the market. We have re-imagined the next generation of Clinical Decision Support (CDS) for health care providers. Traditionally, CDS either lives inside or outside of a hospital’s electronic medical record (EMR). Inside-the-EMR solutions are best described as pop-up alerts that may appear while a provider is accomplishing another task or thinking through a patient’s problem. These pop-up alerts can irritate nurses and physicians, causing “alert fatigue.” Outside-the-EMR support delivers evidence-based content through traditional reference articles that are five to fifteen pages long and can take valuable time to read.
The competitive advantage of the Redivus Health solution is its simplicity and intuitive user experience. National clinical guidelines for treating a critical medical situation like cardiac arrest amount to a complex 30+ step algorithm or multiple pages of PDFs. In a medical crisis, there’s no time to waste. The Redivus platform is quickly accessible on a mobile device. We have taken rather complex clinical algorithms and intelligently automated them so that providers can get through a cardiac arrest, stroke, sepsis, or heart attack event with 100% compliance and documentation accuracy. A great comparison is to GPS apps—what you would expect to see if you launched a cardiac arrest scenario on the Redivus app is similar to the turn-by-turn guidance that a navigational application gives a user to get from point A to point B.
Does this integrate with existing EMR? Is the tool designed to reduce any “screen-time overload” that providers complain of when dealing with EHR systems?
Yes, we can integrate directly with the EMR or use a middleware solution for more rapid integration. The wonderful thing about the solution is as you take your journey through the evidence-based steps, it documents everything in real time, which leads to greater efficiencies and less time-consuming data entry.
Can a tool like this help hospitals and health systems improve their reimbursements?
The short answer is “yes.” We are finding with one of our larger clients that using our tool with Sepsis Surveillance has increased the identification two-fold. Pneumonia vs Pneumonia with sepsis billed by a hospital has a $5000 per case reimbursement difference. This also means that patients are receiving the life-saving treatment sooner, leading to less time in the hospital. Decreased length of stay saves money as well. So, there is a doubling effect of higher revenue and less cost associated with each case.
Can this tool help cut down on medical error, over-treatment, and low value care?
Yes, the Redivus app essentially takes nationally proven guidelines and gives a provider a simple and intuitive way to follow those guidelines. This is the 3D health care checklist, which decreases medical error, limits wasteful treatment, and increases the value of diagnosis and treatment.
Do hospitals currently use the tool?
Yes, our tool is launched 40 times a day on average at 14 different sites, and our customer base is growing rapidly.
Does Redivus collect data on whether or not users are following the treatment decision support given by the tool? Is this data used for HEOR?
Yes, the data is collected by an AWS HIPAA compliant database that identifies the patient data so clinical insights can be gathered.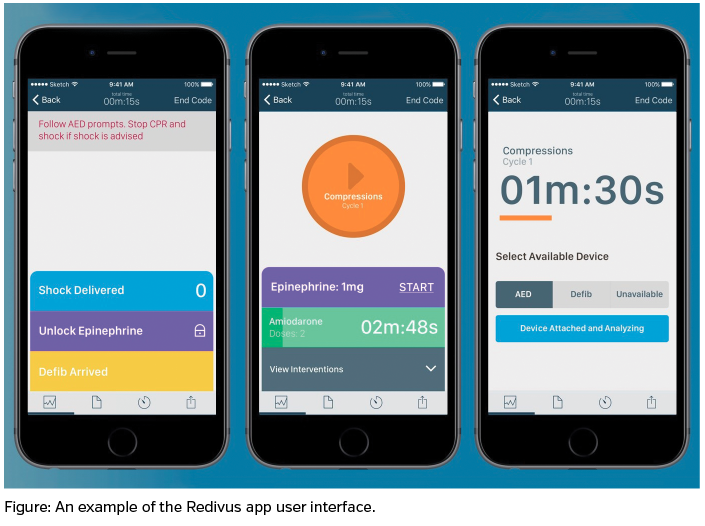
Can you give an anecdotal example of a situation where a tool like this improved outcomes? Do you have any data related to this you can share?
A good recent example comes from Dr. Marc Larsen, an ER doctor who regularly uses the Redivus app. He says they may see five to ten cardiac arrests each month, but even with running codes frequently, he believes the application can make a difference in patient outcomes and helps him save more lives. Doctors like him often credit the app with helping them remain focused and bringing calm to a chaotic situation.
Additionally, we have seen how our app is vital in diagnosing sepsis. At a large health care system, we have screened about 1300 patients that are being transferred from rural America into an urban system. From this process our evidence-based CDS platform has standardized a screening process for sepsis and led to 125 patients being diagnosed before transfer. We have given these patients the term “sepsis saves.”
Are there any other cost-saving or spending benefits associated with the Redivus tool?
Yes, we believe that our tool is not only a diagnostic and treatment adjunct, but also an educational tool. We have found that providers practice the evidence-based steps with the tool, so when they have a real patient they are fluid and fully understand how to execute using the app.
Do clinical pathways have a role in the development or use of the Redivus tool? If so, how?
We currently use nationally-based clinical algorithms by the AHA and the Surviving Sepsis Campaign to feed the logic in our tool and algorithms. As data is aggregated in our tool the more usage will be used to form modifications to those pathways in a data-driven manner. AI/Machine Learning is very much on our road map, and we imagine that it will be incorporated to make our platform smarter, more insightful, and more effective going forward.
Can you explain how medical simulation improves decision support?
We believe that the most effective way to educate and train health care providers is in a simulation setting. High stakes, with low patient risk, should be the gold standard for providers to learn what to do and not do in a medical emergency. We also believe that this is a place that can test the effectiveness and usability of software before using it on actual human beings. Both current methods of decision support are lacking effectiveness because they weren’t fully vetted and tested in simulated settings. Medical simulation is the future of health care, and we intend to continue incorporating it into our training and the testing of our platform.
Are there any other ways decision-support tools can help payers and health systems?
Medical error is the third leading cause of death in the United States today. It is a dire issue that needs to be taken seriously. There is so much that can be done to prevent these errors with better clinical decision support and electronic documentation. Our mission at Redivus is to reduce medical error by improving provider performance and compliance through more manageable and accessible CDS.










