Coprescribing Clarithromycin and a Calcium-Channel Blocker Increases Risk of Hospitalization in Older Patients
New evidence shows that the use of clarithromycin in older adults who are already taking calcium-channel blockers significantly increases a patient's risk of hospitalization and acute kidney injury (AKI) when compared with older adults who were coprescribed the azithromycin and a calcium-channel blocker. This new evidence was presented in a population-based, retrospective cohort study, recently published in Journal of the American Medical Association [DOI:10.1001/jama.2013.282426].
According to the study, clarithromycin and erythromycin are commonly prescribed macrolide antibiotics; however, these drugs are also inhibitors of the cytochrome P450 3A4 (CYP3A4; EC 1.14.13.97) enzyme. Coprescribing clarithromycin and a calcium-channel blocker could lead to serious drug interactions, because calcium-channel blockers are metabolized by the same enzyme. When these 2 drugs are combined, it could lead to blood concentration levels that could be harmful to the patient. A possible alternative is azithromycin, which is not a CYP3A4 inhibitor.
In this retrospective study conducted in Ontario, Canada, researchers studied the risk of acute adverse events after coprescribing clarithromycin and a calcium-channel blocker in older adults. This was then compared to the use of azithromycin and a calcium-channel blocker in an older population.
Robust healthcare databases were used to identify 190,309 older adults who were newly prescribed either clarithromycin (n=96,226) or azithromycin (n=94,083) who were also taking a calcium-channel blocker between 2003 and 2012. Due to the study's location in Ontario, residents had universal access to hospital care and physician services, and patients ≥65 years also had universal prescription coverage.
The mean age of patients in the study was 76 years. The researchers evaluated adverse events that occurred within 30 days of a coprescription index date.
The primary outcome of the study was identified as hospitalization with AKI. Other outcomes of the study were hospitalization with hypotension and all-cause mortality.
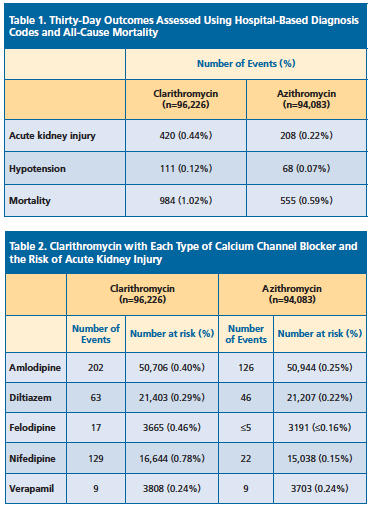
Researchers found that using clarithromycin with a calcium-channel blocker significantly increased the risk of the primary outcome compared to those patients taking both azithromycin and a calcium-channel blocker (See Table 1 below). According to the data, coprescribing clarithromycin and a calcium-channel blocker resulted in a 0.22% higher incidence of hospitalization with AKI.
When researchers assessed the results based on the type of calcium-channel blocker, they found that the highest risk of hospitalization for AKI was for patients who were taking nifedipine (See Table 2 below).
A clarithromycin prescription along with a calcium-channel blocker was also associated with a higher risk of hospitalization with hypotension. Researchers reported that 111 patients who were taking clarithromycin were hospitalized with hypotension compared to 68 patients taking azithromycin (absolute risk increase, 0.04%; 95% confidence interval [CI], 0.02%-0.07%; odds ratio [OR], 1.60; 95% CI, 1.18-2.16).
In addition, the combination of clarithromycin and a calcium-channel blocker was also associated with an increased risk for all-cause mortality (964 patients) compared to those taking azithromycin (555 patients; absolute risk increase, 0.43%; 95% CI, 0.35%-0.51%; OR, 1.74; 95% CI, 1.57-1.93).
While researchers believe the results of their study support current safety warnings regarding the concurrent use of CYP3A4 inhibitors and calcium-channel blockers, they also acknowledged study limitations. For instance, the observation design of the study may not take into account unknown factors. Due to the study population, the results can only be generalized to older adults.