ADVERTISEMENT
The Battle Against Antibiotic Resistance Heats Up
Antibiotic resistance has been referred to as the “public health’s ticking time bomb” and the “next pandemic.” The World Health Organization calls antibiotic-resistant infections one of the biggest threats to global health today.
__________________________________________________________________________________________________________________________________
Related Content:
Obama to Propose Sharp Increase in Antibiotic Funding
Antiobiotic Self-Stewardship Program Improves Targeted Antibiotic Use
__________________________________________________________________________________________________________________________________
The Global Threat
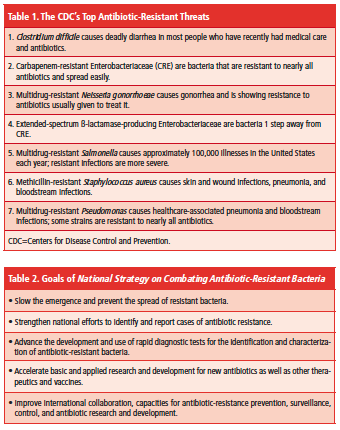
Antibiotics and similar drugs—referred to under the umbrella of antimicrobial agents—have been commonly used to treat infections and diseases for the past 70 years. However, their common use has caused some bacteria to mutate and become resistant to these drugs, according to the Centers for Disease Control and Prevention (CDC). Table 1 lists the CDC’s top 7 antibiotic-resistant threats.
Drug-resistant infections will cost the world 10 million additional deaths each year and up to $100 trillion by 2050 if the global increase is not stopped, according to a major report released in November 2014 from the Review on Antimicrobial Resistance, titled Antimicrobial Resistance: Tackling a Crisis for the Health and Wealth of Nations. The CDC reports that in the United States alone, antibiotic-resistant bacteria infect >2 million people each year, killing 23,000 of them. In addition, almost 250,000 people each year require hospital care for Clostridium difficile (C diff) infections. In most of these infections, the use of antibiotics was a major contributing factor leading to the illness. At least 14,000 people die each year in the United States from C diff infections, many of which could have been prevented.
Antibiotic-resistant infections add considerable and avoidable costs to the US healthcare system. In most cases, antibiotic-resistant infections require prolonged and/or costlier treatments, extend hospital stays, necessitate additional doctor visits and healthcare use, and result in greater disability and death compared with infections that are easily treatable with antibiotics, according to the CDC’s 2013 report Antibiotic Resistance Threats in the United States. While the CDC noted that the total cost of antibiotic resistance to the US economy has been difficult to calculate, the report referenced a 2009 study that showed excess direct healthcare costs as high as $20 billion, with additional costs to society for lost productivity as high as $35 billion annually (based on 2008 dollars) [Clin Infect Dis. 2009;49(8):1175-1184].
Initiatives to Fight Superbugs
“Detecting, preventing, and controlling antibiotic resistance requires a strategic, coordinated, and sustained effort,” said Thomas Frieden, MD, MPH, director, CDC. “Fighting antibiotic resistance is both a public and national security priority.”
In September 2014, President Barack Obama’s administration announced a comprehensive set of new federal actions to combat the rise of antibiotic-resistant bacteria and protect public health. President Obama signed an executive order directing the federal government to work domestically and internationally to reduce the emergence and spread of antibiotic-resistant bacteria and to help ensure the continued availability of effective treatments for bacterial infections. In addition, the administration released its National Strategy on Combating Antibiotic-Resistant Bacteria, a 5-year plan to prevent and contain outbreaks and develop the next generation of tests, antibiotics, and vaccines. The plan outlined 5 interrelated national goals to be achieved by 2020 (Table 2). In addition, President Obama’s Council of Advisors on Science and Technology released a related report on Combating Antibiotic Resistance. The 3 main components of the report include:
(1) Improved surveillance of antibiotic-resistant bacteria to enable effective response, stop outbreaks, and limit the spread of antibiotic-resistant organisms
(2) Increased longevity of current and new antibiotics by promoting appropriate use, preventing the spread of antibiotic-resistant bacteria, and increasing the use of proven interventions to decrease the rate at which microbes develop resistance
(3) Increased rates of discovery and development of new antibiotics
A $20 million prize for the development of a new rapid, point-of-care diagnostic test for healthcare providers to use to identify highly resistant bacterial infections was also launched. The
National Institutes of Health and Biomedical Advanced Research and Development Authority are cosponsoring the prize.
The CDC is also ramping up its efforts to tackle the country’s biggest drug-resistant threats. For the first time, in its 2013 report, the CDC classified drug-resistant superbugs by how dangerous they were. They were ranked “urgent,” “serious,” and “concerning” based on how many people get sick, the number of hospitalizations, and how many deaths were attributed to each. The CDC’s Detect and Protect Against Antibiotic Resistance Initiative (known as the AR Initiative) is part of a broader strategy to target investment aimed at antibiotic resistance. The agency identified 4 core actions to be addressed:
(1) Detect and track patterns of antibiotic resistance
(2) Respond to outbreaks involving antibiotic-resistant bacteria
(3) Prevent infections from occurring and resistant bacteria from spreading
(4) Discover new antibiotics and diagnostic tests for resistant bacteria
One important strategy in fighting antibiotic resistance is antibiotic stewardship to improve prescribing practices and promote more judicious antimicrobial agent use. Numerous studies have shown that implementing an antibiotic stewardship program not only saves lives, but can save significant healthcare expenditures. A University of Maryland study showed that the implementation of 1 antibiotic stewardship program saved $17 million over 8 years at an institution. After the program was discontinued, antibiotic costs increased $1 million in the first year (an increase of 23%) and continued to increase the following year.
A recent retrospective analysis of C diff infections highlighted the need for antibiotic stewardship programs [Am J Infect Control. 2014;42(10):1028-1032]. Researchers analyzed 10 years of data from the US National Hospital Discharges Surveys and found that C diff infections nearly doubled from 2001 to 2010 in US hospitals. Rates of C diff infections among hospitalized adults rose from 4.5 C diff infection discharges per 1000 total adult discharges in 2001 to 8.2 C diff infection discharges per 1000 total adult discharges in 2010. “Antimicrobial stewardship is one of the most important strategies for preventing [C diff infection],” the researchers noted.
Meanwhile, scientists are urgently working to develop new antibiotics that are resistant to bacteria, and research published recently in Nature showed promise [2015;517(7535):455-459]. Uncultured bacteria comprise approximately 99% of all species in external environments and are an untapped source of new antibiotics, according to researchers at Northeastern University. Most antibiotics are produced by bacteria found in the soil; however, only 1% of these organisms can be grown in the laboratory. This led the researchers to take a different approach. Instead of trying to determine what to put in a petri dish, they placed the bacteria directly into the soil, isolating 50,000 different specimens, which made 25 new antibiotics. One compound they called teixobactin, killed certain drug-resistant bacteria including Staphylococcus aureus and Mycobacterium tuberculosis.
Although the research has only been conducted in mice thus far and is a few years from human trials, “the properties of this compound suggest a path toward developing antibiotics that are likely to avoid development of resistance,” the researchers concluded.—Eileen Koutnik-Fotopoulos