Assessing the Cost Burden of AF and Heart Failure
Common complications of acute coronary syndrome (ACS) are atrial fibrillation (AF) and heart failure, and studies have shown that AF and heart failure exhibit the same risk factors. When a patient has 1 complication and then develops the other, there is an increased possibility of mortality.
A recent study used data from the Medicare Beneficiary Survey between 2001 to 2006 [BMC Health Serv Res. 2014;14(1):80]. The Medicare Beneficiary Survey was constructed to represent all Medicare beneficiaries (approximately 16,000) and assess factors with regard to patient’s socioeconomic situation, healthcare resource utilization, and costs.
The sample of individuals with ACS was chosen based on inpatient medical claims in addition to a diagnosis of ACS. The patient characteristics assessed included demographics and socioeconomic factors (ie, age, gender, race, area of residence, employment status, education status, income level, martial status, and living arrangement). Both Medicare claims and survey responses were used to report total healthcare costs. Factored into the healthcare costs were Medicare reimbursements, non-Medicare reimbursements, costs of plan paid, and beneficiary out-of-pocket payments.
The researchers compared AF verses non-AF beneficiaries and heart failure verses nonheart failure beneficiaries. Over the course of 58 months, 795 patients were identified as having ACS, of which 13.1% had AF and 22.9% had heart failure. The study revealed individuals with heart failure were older (78.5 years vs 75.4 years), more likely to be institutionalized (14% vs 4%), or more likely to be diagnosed with hypertension (78% vs 65%), and less likely to be currently employed (1.6% vs 9.9%) than AF patients.
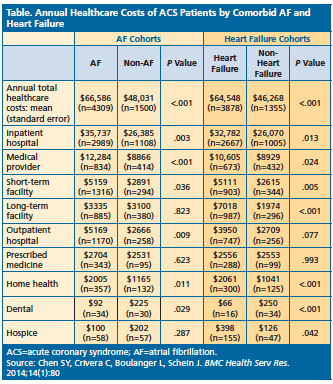
In terms of annual total healthcare, ACS patients with AF had a significantly higher mean cost of $66,586, while ACS patients without AF had a mean cost of $48,031. The major influences on costs for AF and non-AF patients were inpatient hospital costs ($35,737 vs $26,385) and medical provider costs ($12,284 vs $8866).
ACS patients with heart failure also had higher total costs than patients without heart failure ($64,548 vs $46,268). The main cost drivers for heart failure beneficiaries versus nonheart failure patients were inpatient hospital ($32,782 vs $26,070) and medical provider costs ($10,605 vs $8929). See Table below for annual healthcare costs.
Both AF and heart failure patients have a much lower probability of survival compared to patients without AF and heart failure (P=.001). Beneficiaries with heart failure had a 41% higher risk of mortality after adjusting for patient demographics and socioeconomic factors.
ACS patients with AF had healthcare costs that were 1.21 times the cost of individuals without AF (P=.008). ACS patients that had heart failure incurred healthcare costs the were 1.25 times the cost of patients without heart failure (P=.001). To improve outcomes and quality of care for patients with AF and heart failure, interventions and cost-effective strategies should be implemented, according to the researchers.