Accurate, Inexpensive Risk Prediction Tools Needed to Justify Tailored Colorectal Cancer Screening
Washington, DC—Modest misclassification rates and costs of risk prediction tools substantially impacted the effectiveness and cost-effectiveness of tailored screening for colorectal cancer (CRC) compared with standard screening recommendations, according to results of sensitivity analyses presented during Digestive Disease Week by Uri Ladabaum, MD, professor of medicine, gastroenterology and hepatology, Stanford University.
Individuals considered to be of average risk for CRC likely include a spectrum of risk, thus tailoring screening has been seen as a strategy to potentially improve effectiveness as well as cost-effectiveness. Although CRC risk prediction tools having modest discriminatory ability exist, they are not widely used. “One of the problems is you never really know what an individual’s actual risk is,” Dr Ladabaum said, “so the question becomes, how good is the tool and does it cost anything?”
Dr Ladabaum and colleagues adapted a validated decision analytic model of CRC screening to explore the potential effectiveness and cost-effectiveness of tailored CRC screening based on the results of a prediction tool (consisting of an algorithm, biomarker, or combination); and examine the influence of the tool on discriminatory ability and cost.
Researchers used a Markov cohort model, which they recalibrated to reflect a spectrum of lower, average, and higher risk of CRC. Different screening strategies were applied for different predicted risk levels defined by the risk tool. The age of the screening population was 50 to 80 years.
The researchers compared tailored screening with usual screening for effectiveness (quality-adjusted life-years [QALYs]/ person) and cost-effectiveness (cost/ QALY gained) using 2 scenarios.
The first scenario compared tailored colonoscopy with either colonoscopy every 10 years for all patients starting at age 50; colonoscopy once at age 60 for those at lower risk; colonoscopy every 10 years for those at mid risk; or colonoscopy every 5 years for those at higher risk. The second involved a strategy of tailored fecal immuno- chemical testing (FIT) for almost all patients, with colonoscopy offered to those considered at higher risk. Specifically, those at lower and mid risk were given FIT yearly, with colonoscopy offered in addition every 5 years for those at higher risk.
The researchers defined “lower risk” as a lifetime risk of ≥3% after 50 years of age; if risk was ≥12%, patients were considered higher risk. Coincidentally, Dr Ladabaum said, the lower-risk threshold represented about half of what is considered average risk and the higher-risk threshold, about 2 times average risk.
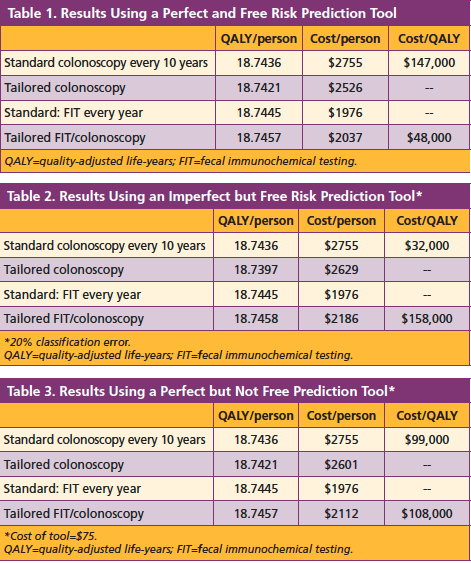
Results of their base case, which assumed the prediction tool was perfect and free, showed that a strategy of tailored colonoscopy vs performing the standard recommendation of colonoscopy every 10 years was slightly less effective, but was more cost-effective, saving $147,000/ QALY (Table 1). The strategy of tailored FIT with colonoscopy showed more effectiveness and although slightly more costly, resulted in a gain of $48,000/ QALY.
The results of the first sensitivity analysis assumed the risk prediction tool was not perfect, but free (Table 2). In this analysis, it was assumed the tool had a 20% classification error, and demonstrated the standard approach to be more cost-effective than the tailored strategies.
The results of the second sensitivity analysis assumed the risk prediction tool was perfect, but had a cost of $75 (Table 3). The researchers found that the effectiveness for the tailored colonoscopy strategy did not change but cost increased; effectiveness increased slightly for the tailored FIT strategy but also did not show cost-effectiveness.
In conclusion, Dr Ladabaum said that the use of a highly accurate and inexpensive CRC risk prediction tool could yield savings with a minimal decrease in effectiveness when used to tailor colonoscopic screening. Further, it could lead to improved effectiveness at acceptable costs when used to shift higher-risk persons in a FIT program to a strategy of colonoscopy every 5 years.—Mary Mihalovic