10 Years Since ACOs were Implemented: How Far Have They Come?
Las Vegas—The first accountable care organizations (ACOs) were implemented in 2005, beginning with just 10 large multispecialty groups of approximately 5000 physicians. Since then, the idea has been widely debated and ultimately encouraged under the Patient Protection and Affordable Care Act (ACA).
During a session at the NAMCP forum, Jane DuBose, senior director, Decision Resources Group, discussed the evolution of ACOs and how the ACA has changed the process.
Background on ACOs
The guiding principles of an ACO include [Health Aff. 2010;29(5):982-990]:
• Provider-led organizations with a strong base of primary care providers (PCPs) that are collectively accountable for quality and total per capita costs across the full continuum of care for a patient population
• Payments are linked to quality improvements that also reduce cost
• Reliable and progressively more sophisticated performance measures to support improvement and provide confidence that savings are achieved through improved care
According to the presentation, as of the fourth quarter of 2014, more than 840 separate ACO contracts had been counted, involving patients insured by commercial, Medicaid, and Medicare payers. As of data from October 2014, California, Florida, and Massachusetts have the highest number of ACOs, with more than 31 ACOs in each state. Conversely, the states that still have not adopted ACOs include Alaska, Hawaii, Delaware, South Dakota, and Wyoming.
Ms. DuBose explained the changing landscape of ACOs from 2014 to 2015, including:
• Integrated delivery networks and advanced medical groups are entering the ACO market and taking more risks for quality incentive and outcomes-based rewards
• Medicare is moving away from the fee-for-service payment model and experimenting with new options to manage beneficiaries
• Health plans and providers are merging to survive reimbursement cuts
• New types of partnerships between medical groups, managed care, and hospitals are emerging
Different Programs
Ms. DuBose noted that 50.2% of ACOs are commercial payers, 42.9% are Medicare payers, and 5.9% are a combination of payers. At the time of the presentation, there were 340 Medicare Shared Savings Programs (MSSPs), including 19 Pioneer ACOs, which was down from 32 programs in 2012. MSSPs must have a minimum of 5000 beneficiaries, while Pioneer programs must have 15,000 beneficiaries. In addition, there were approximately 53 Medicaid ACOs operating or in development in 11 states. States have not set minimum patient requirements for these types of ACOs. In the commercial space, 426 performance-based or shared savings contracts were established between payers and provider groups. Commercial ACOs are required to have anywhere from 5000 to 100,000 covered lives in a single ACO.
Gains and Losses
The first year results for MSSPs proved to be underwhelming. Of the MSSPs operating in 2012, only one-fourth, or 50 out of 223, achieved savings on their assigned beneficiaries. The largest gain, of $57.83 million, was seen at Memorial Hermann Healthcare System in Houston, Texas.
Pioneer programs have also been struggling, as a number of programs have dropped out, citing difficulty in realizing savings based on the Centers for Medicare & Medicaid Services (CMS) benchmark methodology. Pioneer programs also carry more risk, transitioning to a shared-risk and shared-loss model for the current performance year.
However, Pioneer programs improved on 28 of 33 quality measures from year 1 to year 2, according to Ms. DuBose. Of the 23 ACOs that remained in the program for year 2, all but 1 improved the overall quality score, though higher quality scores do not necessarily correlate to higher financial rewards, she noted. The largest improvements were seen in the at-risk population, jumping from an average quality score of 67.5% in year 1 to 83% in year 2. This group is important to the core of ACOs, as managing chronic diseases is often difficult and costly.
Nearly 30% of ACOs are physician-controlled, while more than 100 ACOs are jointed guided by payers and
physicians. Ms. DuBose compared how physician-led Pioneer programs held up against health-system led programs. For physician-led programs, 3 out of 6 saw savings, while 8 out of 14 health system-led programs had savings.
Looking Ahead
Despite the mixed results of the Pioneer programs, Ms. DuBose expects more Pioneer groups will be named by the CMS this year. Providers are still concerned about the potential for loss in these groups, asking that financial rewards be larger, suggesting patients be able to choose their ACO rather than be attributed through their PCPs, and questioning the way benchmarks are used for computing financial gains or losses.
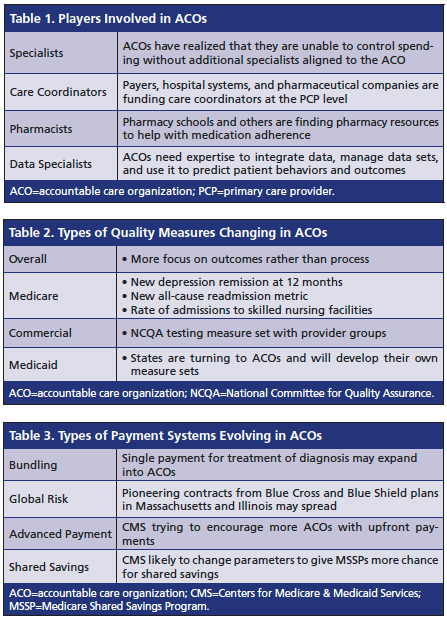
Ms. DuBose closed the session by examining the future of ACOs, including expanding players (Table 1), changing quality measures (Table 2), and evolving payment systems (Table 3).
In addition, Ms. DuBose noted that patient engagement will need to be improved, particularly in more complex patients, including those with end-stage renal disease, cancer, and other rare diseases. She also speculated that hospital-owned practices will be more likely to be clinically integrated and/or involved in ACOs, as mergers will tilt more practices into organized models. Payers will continue to focus on value, not volume-based reimbursement.—Kerri Fitzgerald