The Patient-Centered Medical Home of the Future
 FRMC: Can you describe some of the benefits offered by the Patient-Centered Medical Home (PCMH) and the Patient-Centered Specialty Practice (PCSP) Recognition programs to payers, providers, and patients?
FRMC: Can you describe some of the benefits offered by the Patient-Centered Medical Home (PCMH) and the Patient-Centered Specialty Practice (PCSP) Recognition programs to payers, providers, and patients?
The original intent of the PCMH model—as described in the Joint Principles of the PCMH (American Academy of Family Physicians; 2007)—was to describe and advocate for a way of practicing primary care that returned the focus to delivering care in a highly organized, safe, timely, efficient, effective, equitable, and patient-centered manner (ie, according to the Institute of Medicine’s six aims from Crossing the Quality Chasm: A New Health System for the 21st Century [National Academies Press; 2001]). The concept of the “medical neighborhood,” described in a position paper by the American College of Physicians (The Patient-Centered Medical Home Neighbor: The Interface of The Patient-Centered Medical Home With Specialty/Subspecialty Practices; 2010) led to the creation of the PCSP Recognition program by NCQA.
These two programs align very well and address the core elements of what leads to a high-performing practice. For medical specialists, the emphasis is less on longitudinal care and more on coordination and collaboration with referring practices—though clearly longitudinal relationships do exist within the specialty of oncology. In fact, in some cases, and especially in oncology, specialists do become the primary care physicians for their patients. Hopefully, this is a dynamic situation in that oncologists may return people to their primary care physicians once a person is cured or in remission.
It is clear that when practices transform and adhere to the PCMH model of care, the evidence suggests that quality improves, inappropriate and avoidable costs are reduced, clinicians experience less burnout, and people have a better experience. To make the transformation, practices need technical and financial support provided over a period of time sufficient to make the changes and anchor them in the culture of the organization.
Although we do not have comparable research on the PCSP Recognition programs, it is reasonable to expect that these same factors would contribute to success in specialty practices.
FRMC: In the recent redesign of the PCMH Recognition program, the biggest change seemed to be a shift from fully documented review every 3 years to virtual check-ins occurring annually. Why did NCQA feel this was a better format for PCMH?
The change from a 3-year cycle to initial recognition followed by annual check-ins was driven by several factors. We heard from key stakeholders that the performance of recognized practices sometimes regressed during the interval between renewal of their recognition status. Instituting the annual reporting requirement will help ensure that practices continue to pay attention to the key aspects of the PCMH model. More importantly, we believe that this new process will ultimately reduce the work involved in the recognition process because the requirements for sustaining recognition (ie, the annual reporting) will be significantly streamlined. We intend to provide choices for how practices can demonstrate aligned ongoing adherence to the program. The intent is to check on some fundamental aspects of the PCMH model that, if met, indicate that the practice is continuing to deliver patient-centered primary care. NCQA will also audit a minimum of 5% of practices’ submissions.
FRMC: What are some of the other key changes you’ve made to the program, and what shortcomings of the original design do you hope these changes address?
We believe the new process will address most—if not all—key concerns we heard during the focus groups that helped inform the redesign effort. For example, some of the issues we heard were that the previous effort:
• was too difficult for small practices;
• focused on process instead of performance;
• required too much documentation;
• provided too little contact with a real person at NCQA;
• allowed momentum to decline within the practice during the lengthy 3-year period before renewal;
• failed to inform practices of their submission’s status or need for revisions in a timely manner; and
• provided too little education and guidance.
In addition to moving to an initial recognition followed by annual check-ins, the following are some of the other key changes:
• For the first time, we will assign each practice seeking recognition to a specific NCQA staff person. NCQA staff will support the recognition process by scheduling the check-ins, facilitate the selection of criteria to be satisfied at each check-in with an evaluator, coordinate the check-ins, and be the single point of contact for the practice.
• We designed the new Recognition platform to be as intuitive as possible, with clear indicators of progress, pending work, tasks to complete, and explanations of the criteria and evidence needed to meet the criteria.
• We reduced the documentation requirements. Instead of sending reams of documentation, practices will have the option of actually showing the reviewer the process through virtual screen-sharing during a live review.
• We plan to create short videos and other instructive material for the new platform. We have developed new education programs for recognized practices (such as “Strategies for Success as a PCMH, available at www.ncqa.org/pcmhstrategies), and will embed links to other NCQA educational content over time in the new platform.
FRMC: In particular, there seems to be some concern regarding practices’ ability to measure many key processes and data using current electronic medical records (EHR) and health information technology (IT) systems. Will it be possible for practices to meet the standards of the PCMH model without upgrading these systems? Or will recognition attempts require complete overhauls in some cases?
Practices will not need to do any significant upgrades to their EHR or health IT systems solely for the upcoming PCMH standards or the new Recognition process. We plan to introduce an option in 2017 for PCMH practices to electronically submit the results of clinical quality measures in lieu of documenting some quality-related activities required in the PCMH standards. The measure set from which practices will be able to choose is aligned with the EHR Incentive Program measures (also known as “Meaningful Use”). NCQA is currently engaged in discussions with several health IT vendors through which practices will be able to submit these measures. More details will be forthcoming.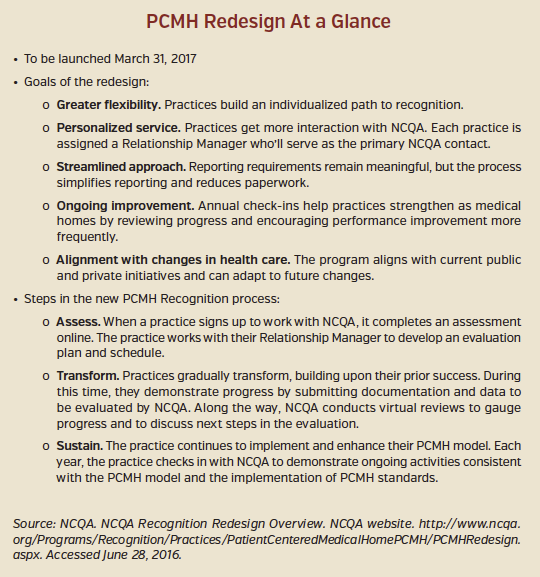
If practices elect to submit electronic clinical quality measures, they may have to work with their health IT vendor to facilitate that data flow; however, this will be an optional reporting method that we hope will wind up saving practices time and effort.
NCQA’s health IT pre-validation program helps to identify technology vendors that have tested their systems against NCQA criteria. Practices that implement these solutions generally are able to get auto-credit towards some elements/factors in the recognition process depending on what the vendor tested against.
In future years, we hope to test health IT systems’ capabilities to submit metadata about workflow processes (eg, test tracking, turnaround time for online patient inquiries). However, much more work needs to be done before this is a reasonable option.
FRMC: Do you expect to make any more changes to the system as you receive feedback from stakeholders?
Just as in any good quality improvement project, we expect to learn as the implementation proceeds and make appropriate adjustments. The PCMH community has been extremely helpful and supportive when we solicited feedback, and we hope/expect that to continue. Our experience with the launch of the PCMH program will be critical to the successful migration of the PCSP Recognition program in 2018.












