Opioid Addiction Treatment: Can Managed Care Make an Impact?
In an open letter recently sent to all physicians, US Surgeon General, Vivek Murthy, MD, pleaded for help with solving America’s opioid crisis. He wrote that since 1999, overdose deaths from opioids have quadrupled and prescriptions for the pain management drugs are so prevalent that every American adult could have a bottle.
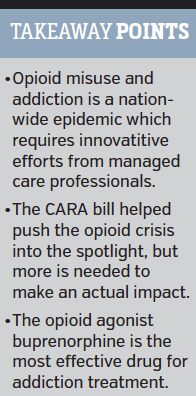
In 2012, health care providers wrote 259 million prescriptions for opioid pain medications, according to Centers for Disease Control and Prevention (CDC) data. Opioid abuse is being called a national epidemic, and experts say it will take multiple stakeholders, including managed care organizations, to curb its effects and reverse the growing trend of misuse.
Legislators, providers, payers, and government organizations are all taking steps to try to address the growing problem of opioid misuse. The data surrounding opioid abuse is staggering, with the White House reporting that more Americans are now dying from drug overdoses than motor vehicle accidents each year. It's a problem that has immense impact on the individuals and families directly involved while also taking a significant toll on the US health care system.
FAIR Health, a national, independent, nonprofit organization with access to more than 20 billion privately billed health care claims, recently released a white paper showing that between 2007 and 2014 the number of privately billed claim lines with an opioid dependence diagnosis rose by 3203%.
"I think why this study has garnered so much attention is because it peels back the curtain on the private health care market," Robin Gelburd, JD, president of FAIR Health, said in an interview.
Ms Gelburd stated that the 3203% increase reflects the number of services rendered to people who had an opioid dependence diagnosis during that time period. The study also found that the number of claim lines that had a pregnancy drug dependence diagnosis also increased by 511% between 2007 and 2014.
"We are hoping a number of researchers and policy makers can take this data and start really trying to uncover the dynamics giving rise to these increases," she said.
Furthermore, in a more recent FAIR Health report, researchers found that health spending on opioid dependence increased by 1375% between 2011 and 2015, from $32 million to $446 million.
According to Ms Gelburd, the company released these reports in hopes of moving the issue from an individual level to a macro level by showing just how significant the impact is on health care resources.
"This should be of obvious concern to all of us," she said.
Compromising Legislation
The opioid abuse epidemic has also caught the attention of lawmakers who made several efforts this summer to expand opioid misuse treatment options.
US President Barack Obama signed the Comprehensive Addiction and Recovery Act of 2016 (CARA) into law in July, authorizing $181 million in new spending to create new treatment programs and expand current treatment efforts. However, the act fell short of President Obama's initial goal of more than $1 billion in relief funds, severely compromising the bill’s efforts.
Andrew Kolodny, MD, executive director of Physicians for Responsible Opioid Prescribing, said that while he's pleased the bill passed, overall the final product did not include many of the aspects that would have been most helpful in addressing opioid addiction.
"The CARA bill didn't include any funding to expand access to treatment; there was an effort to get some funding put into it that got rejected,” Dr Kolodny said. “So right now CARA as is, will have a very limited impact.”
He said that he believes the most helpful aspect of the act will be that it removes prohibition against nurse practitioners and physicians assistants from prescribing buprenorphine, a partial opioid agonist commonly used to treat opioid addiction.
"The bill set up a mechanism for nurse practitioners and physicians assistants to become eligible to become buprenorphine prescribers, which I think is very helpful," he said
In August, a new rule from the Substance Abuse and Mental Health Services Administration went into effect that allows doctors to treat more patients with buprenorphine.
Previously, physicians had a 30-patient cap on buprenorphine in their first year of prescribing the drug, along with a 100-patient cap in following years. The new rule allows providers to treat as many as 275 patients simultaneously, if they meet certain criteria.
Caleb Alexander, MD, co-director of the Johns Hopkins Center for Drug Safety and Effectiveness, called the passage of this new rule "great news" but says there are still other barriers in place that hinder patients from getting the addiction treatment they need.
Fighting ADDICTION on two fronts
According to experts, physician efforts to address the problem have become divided into two categories: preventing new patients from becoming addicted and helping those who already are.
Both Dr Alexander and Dr Kolodny said that they believe the problem stems from physicians being too quick to prescribe opioids for pain management.
"Historically, I think we've underestimated the addictive potential of these drugs and at great cost to patients and their loved ones," Dr Alexander said.
He believes physicians need to prescribe opioids more cautiously and cautioned that physicians need to know that abuse-deterrent formulations of opioid medications are not any less addictive.
"Abuse-deterrent formulations are no less addictive than their counterparts, and we've done work suggesting that many providers erroneously believe that they are less addictive," he said.
When it comes to treating patients who are already addicted to opioids, Dr Kolodny says buprenorphine has an effective treatment in randomized clinical trials and should be something more physicians consider.
"If you speak to primary care doctors who actually give it a try, many really like doing opioid addiction treatment with buprenorphine,” he said. “Patients get better pretty quickly in many cases.”
According to Dr Alexander, there is also a large opportunity for providers and health systems to improve their protocols for identifying and treating patients who have an opioid addiction problem.
How Payers Can Help
While a bulk of the attention is often given to those prescribing opioid medications, experts say payers can also play a vital role in curbing abuse and misuse.
"One important role that payers play is in the design of pharmacy and medical benefits that facilitate access to a variety of evidence-based alternatives to prescription opioids," Dr Alexander said.
He explained that if alternative treatments are more difficult for physicians to prescribe, then the less likely they are to end up in the hands of patients, and, instead, physicians will rely on more addictive opioid treatments.
According to Dr Kolodny, one possible misuse prevention strategy for payers is to use the CDC’s Guideline for Prescribing Opioids for Chronic Pain as a resource when developing their policies.
"Managed care companies have an opportunity to look very closely at those CDC recommendations and build policies around them," he said.
For instance, the CDC recommended that acute pain patients rarely need more than 3 days of an opioid, so Dr Kolodny says managed care companies could put into place a prior authorization for prescriptions written for more than 3 days for newly prescribed patients. He said utilizing prior authorizations to make prescribing opioid medication a little more difficult for the physician could help curb its use.
For those patients who already have become addicted, Diana Williams, MSW, behavioral health director for technical assistance at the Altarum Institute, said in an interview that the consulting company has observed positive outcomes when using care coordination, or a care manager, to help people get to the appropriate services.
"Care coordination has been successful in the substance use disorder world, " she said.
The Association for Community Affiliated Plans (ACAP) also examined strategies for reducing prescription drug abuse currently being used at 13 ACAP-member Safety Net Health Plans in a 2015 report. Study findings focused specifically on the efforts’ health plans put into place as the result of an ACAP substance use disorder collaborative with the Open Society Institute aimed at combating the misuse of prescription drugs.
Deborah Kilstein, MBA, vice president of quality management and operational support for ACAP, said that the associations addiction action plans can be a useful resource for those looking to develop better opioid addiction treatment. The ACAP action plans rely on 5 different addiction treatment strategies:
• use of screening, brief intervention, and referral to treatment: a practice that can be used by health care providers, including primary care physicians, that is used to identify, reduce, or avoid drug abuse by asking screening questions and a brief intervention in the office before referrals are made;
• outreach to providers and to members;
• offering specialized support: while all plans had case management programs, several chose to have specialized case management for individuals with substance use disorder;
• initiating or expanding lock-in programs: locking a Medicaid patient into an individual prescriber or pharmacy to receive their medication; and,
• improving the quality of medication-assisted treatment.
Overall, experts agreed that opioid misuse and addiction treatment are issues that require significant effort from the entire spectrum of health care professionals, especially those working in managed care.
“Years from now, I want us to look back and know that, in the face of a crisis that threatened our nation, it was our profession that stepped up and led the way,” US Surgeon General Murthy concluded in his letter. “I know we can succeed because health care is more than an occupation to us. It is a calling rooted in empathy, science, and service to humanity.”










