Opening the Door to a Payment Paradigm Shift
 With specialty drugs expected to account for half of total drug spending by 2018, payers are beginning to target the pricey medications for utilization management, according to Mike Ellis, BS Pharm, chief executive officer, Maxor National Pharmacy Services, Gaithersburg, MD, and Fauzea Hussain, MPH, senior vice president, Avalere Health, Washington, DC.
With specialty drugs expected to account for half of total drug spending by 2018, payers are beginning to target the pricey medications for utilization management, according to Mike Ellis, BS Pharm, chief executive officer, Maxor National Pharmacy Services, Gaithersburg, MD, and Fauzea Hussain, MPH, senior vice president, Avalere Health, Washington, DC.
The pair discussed strategies to manage specialty drugs in current and evolving alternative payment models during a session at the AMCP Managed Care & Specialty Pharmacy Annual Meeting.
Changing times
The growth in the percentage of drug spending going toward specialty drugs is occurring against a changing backdrop. Payment and delivery models are undergoing a profound paradigm shift, as a fee-for-service approach and its emphasis on volume takes a backseat to alternative payment models and their focus on value.
Both public and private sectors have announced unprecedented goals to migrate to alternative payment models, the presenters explained. The US Department of Health and Human Services plans to shift half of all Medicare fee-for-service payments to alternative value-based models by 2018. Meanwhile, payers, providers, and other thought leaders serving on the Health Care Transformation Task Force have committed to putting three-quarters of their business into alternative payment models by 2020.
A Look at Alternative Payment Models
The presentation covered 5 key alternative payment models emerging from health reform: accountable care organizations (ACOs), patient-centered medical homes, bundled payments, medication therapy management, and value-based insurance designs.
To be successful, ACOs must keep costs down while generating positive patient outcomes. While the results of public ACOs have been modest so far, commercial ACOs have shown more promise, according to presenters. Earlier this year, Cigna reported that its ACO collaboration with Brown & Toland Physicians cut outpatient costs 6%, inpatient costs 3%, and professional costs 1% while maintaining quality of care. Overall, the ACO’s medical cost trend was 5.4% lower than the local market.
The presenters also highlighted an ACO partnership between Aetna and the Banner Health Network that reduced medical costs an average 5% per member, while cutting avoidable remissions by 9% and radiology services by 9%. Generic prescribing increased 4%.
The patient-centered medical home model provides primary care practices with a financial incentive to supply and oversee comprehensive and coordinated care for patients. In October 2012, 450 primary care practices began a 4-year initiative administered by the Center for Medicare & Medicaid Innovation (CMMI). During the first 2 years, practices received care management fees per patient in addition to fee-for-service payments. Then, during the second 2 years, shared savings replaced fee-for-service payments. Although the initiative is ongoing, preliminary results suggest it is reducing overall costs while achieving quality measures. 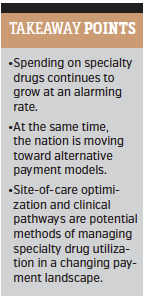
Both public and private payers are trying out bundled payments, which cover an array of services through a single payment. Under CMMI’s Oncology Care Model, which begins when a beneficiary receives chemotherapy and extends out 6 months, practices are eligible to receive up to the difference between target price and actual spending, the presenters explained.
A bundled payment program tested by UnitedHealthcare prospectively paid for an entire course of cancer treatment, regardless of the services or drugs prescribed. Across 5 oncology groups, the effort decreased costs by 34% and saved $33 million.
Enhanced medication therapy management is occurring in the public and commercial marketplace, as CMMI tries out medication therapy management strategies proposed by Part D sponsors and Walgreens’ WellTransitions program is reducing readmissions risk by supporting medication adherence.
CMMI is also set to investigate a Value-Based Insurance Design Model in a handful of states starting next year. The model allows Medicare Advantage plans to offer supplemental benefits or reduced cost sharing to enrollees with certain chronic conditions.
Options for Utilization Management
Payers can use site-of-care optimization and clinical pathways to manage the use of specialty drugs in alternative payment models, the presenters coached. Site-of-care optimization reduces expenses by promoting lower-cost, clinically appropriate settings for administration or infusion.
“Some specialty drugs can be administered at several different sites of care, including hospital
outpatient departments, physician offices, infusion centers, retail clinics, and patients’ homes. For the same service and dosage, however, payment can vary significantly across these sites based on reimbursement methods and approaches to contracting,” the presenters explained.
“Payment rates in hospital outpatient departments can be well past 3 times as high as rates at alternate sites, though the difference varies by drug and setting.”
Clinical pathways can also help control specialty drug use. More prescriptive than clinical practice guidelines, clinical pathways provide specific guidance on the sequence of care.
“Pathways often, although not always, factor the cost of care into treatment decision making,” the presenters said, “and this consideration is likely to expand in the future.”
Clinical pathways standardize care through evidence-based medicine and can be helpful to payers, providers, and patients, according to the session. Pathways offer providers the opportunity to manage risk and improve outcomes — and, in alternative payment models, can even increase their eligibility for financial rewards through better outcomes. For payers, pathways can reduce unnecessary care, cut costs, and even help improve provider performance and achieve quality targets.
For patients, a big upside of clinical pathways is the assurance of care based on gold-standard guidelines. Treatment choices may narrow, the presenters noted, but it is possible many patients will be unaware of a pathway’s influence on their plan of care at all.—Jolynn Tumolo










