Oncology Clinical Trials: A Win-Win for Payers
 As rising prescription medication costs remain a primary concern for many in the medical community, proposed solutions for reining in related spending have ranged from speeding the drug approval process to importing generics from abroad.
As rising prescription medication costs remain a primary concern for many in the medical community, proposed solutions for reining in related spending have ranged from speeding the drug approval process to importing generics from abroad.
At the heart of many of these proposed ideas is the notion of increasing competition among pharmaceutical companies, but this concept may not ring true for those in the oncology sector where new cancer drugs, called checkpoint inhibitors, are making it increasingly difficult to drive down the cost of therapies.
The inhibitors work by allowing the immune system to recognize and attack cancer cells. Bristol-Myers Squibb’s Yervoy (ipilimumab), which treats melanoma by targeting a protein known as CTLA-4, was the first to arrive back in 2011. Although it would be over 3 years before the FDA approved another checkpoint blockade drug, new options began to arrive in late 2014.
Current players include Opdivo (nivolumab; Bristol-Myers Squibb), Keytruda (pembrolizumab; Merck), Tecentriq (atezolizumab; Roche), and Bavencio (avelumab; Pfizer), which all target a protein called PD-1 and have been shown to be helpful in treating several types of cancer. While the drugs are improving survival odds for patients, they also come at a substantial cost.
Existing checkpoint inhibitors each have a list price of nearly $150,000 per year, according to recent a Reuters report, and a combination of Yervoy and Opdivo, approved for patients with advanced or inoperable melanoma, costs over $250,000 a year.
Health insurers have had success negotiating price reductions in some other areas, but discounting is less common for these types of innovative cancer drugs. And every time a more effective drug hits the market, it essentially resets the competition clock. After all, no cancer patient wants the second-best option available.
It is a phenomenon that presents a clear challenge for payers, particularly considering mandates that require the coverage of certain classes of drugs regardless of price. As the search for solutions continues, new ideas and possibilities continue to surface as well.
Clinical Trials as Cost Saver
At the annual Drug Benefit Conference hosted by the Pharmacy Benefit Management Institute (PBMI) March 6 to 8, 2017, Peter Bach, MD, MAPP, director of the Center for Health Policy and Outcomes at the Memorial Sloan Kettering Cancer Center, delivered a presentation focused on the use of comprehensive genomic profiling for managing oncology spending.
During the talk, he pointed out that there are currently some 800 immunotherapy trials going on in the United States, including hundreds in late stage development. When his group last counted, there were 160,000 slots in these studies. It is a phenomenon unlike anything seen before, and this wave of innovation is creating the potential for patients to be matched with trials that suit their needs.
“We’ve never had access to the databases that we do now, in terms of finding patients to put in trials,” he said during the presentation. “This actually ties directly to the issue of drug pricing—it turns out that it is actually a good ‘deal’ from the payer’s perspective to have a patient go on a trial.”
He explained that based on the elimination of high drug costs, clinical trials actually make good fiscal sense for payers. It is an opportunity for savings considering the therapies under investigation are paid for by the trial sponsors. Those drug costs, which amount to 80% of cancer treatment expenses, are thereby avoided or delayed. With an average oncology clinical trial duration of about 8 months, every patient participating in a study can save the payer up to roughly $64,000, according to the presentation.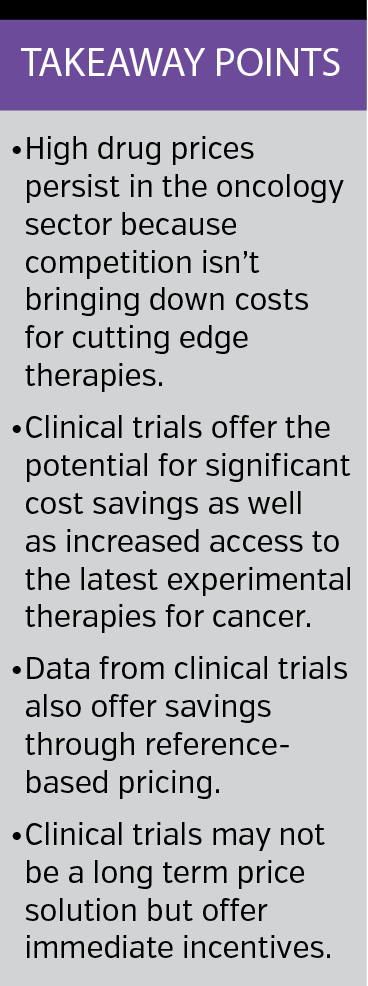
“I would never advocate that as a reason to go into a clinical research study from a payer’s perspective,” Dr Bach clarified. “The reason patients should go into clinical trials is that the trials make sense for them and have good potential and could benefit them and there aren’t other good treatments they are foregoing as a result.”
While not every patient who is tested is placed in a clinical trial, a matching approach can be considered along with the amount one would be willing to pay to reach a breakeven point. With the assumption that a patient placed on a trial is net neutral and net cost and it is possible to get to a matching rate of, say, 8% or 9%, then that point comes at about $6000 per test, according to the presentation.
Again, Dr Bach continually emphasized that he is not advocating for use of clinical trials solely as a cost cutting measure. However, he stated that if cost savings is a “fortuitous consequence” of putting a patient on a clinical trial then “that seems fine because it saves the patient money as well,” because there is no coinsurance on investigational agents.
Could more efficient use of clinical trials benefit patients and payers alike? “That is sort of the last question around personalization which I think hasn’t really been thought through,” he said, “in terms of the larger drug pricing environment.”
Reference-Based Pricing
There are, of course, other ways of looking at clinical research as a means of reducing spending for payers. "If a payer wanted to use data from clinical trials to save money for themselves and still take good care of the patient and still try to understand how to decrease the national overall spending, then the way that they could do it is referenced-based pricing," Thom Walsh, PhD, told First Report Managed Care.
The chief strategy officer and founder of Cardinal Point Healthcare Solutions and adjunct faculty member at the Dartmouth Institute for Health Policy and Clinical Practice pointed out that relying on physicians alone to change their behavior based on clinical trial data does not tend to work. One prime example can be found in the treatment of prostate cancer.
“Patients who receive proton beam therapy don’t live any longer, and they don’t have fewer side effects. It’s just way more expensive,” he said, “but putting that trial data out has not diminished the growth in use of proton beam therapy.”
Providers do respond to changes in financial incentives, however, and payers could design incentives based on findings from clinical trials in the hopes of reducing spending. If evidence shows that two treatments have similar outcomes along with similar side effects but one is more expensive than the other, payers could choose to cover the expense of the treatment that is equally effective but more affordable.
“That is reference-based pricing,” Dr Walsh said. “That makes good sense. You’re not denying anybody good care. You’re just trying to spend money wisely.” Although the idea has been around for a while, from his vantage point it has not been used as widely as one might expect. A large-scale example can be found in the state of Maryland, however, which sets the price that can be charged for a procedure or treatment. “Then the payers and everybody else has to compete around delivering better quality.”
“That is definitely something that we are looking at,” Bhuvana Sagar, MD, national medical director for oncology with Cigna, said of reference-based pricing. She also pointed to a patient decision support tool launched with the intent of making it easier for providers to enter patient information and details about their stage of cancer and type of mutation.
The portal is used to compile clinical information and drive improved adherence to guidelines put forth by the National Comprehensive Cancer Network that are based on expert opinion and clinical trials. “What we’re trying to do is to make sure that the right patient gets the right treatment,” she told First Report Managed Care.
Dr Sagar emphasized the importance of utilizing strategies that have been shown to drive cost savings, such as cutting down on overutilization, addressing underutilization, and making use of patient-centered medical homes. Engaging in shared decision-making is also crucial, she said, to ensure awareness of the prognosis and what it is that patients can truly expect from a drug before they are put on any given treatment regimen.
“The truth is that the wave of innovation that is going on right now has created this other possibility for patients who can get matched to trials,” Dr Bach said during his presentation at the PBMI 2017 Drug Benefit Conference. “There are very few win-wins, and I would never suggest that this is a win-win because... on the backend could be the approval of a new drug that costs a huge amount of money, but at least in the instant... the math [works out].”










