Insulin Therapies: What is Behind the Escalating Cost?
According to Centers for Disease Control and Prevention reports, more than 29 million Americans have diabetes, with the overwhelming majority of cases (90% to 95%) being type 2 diabetes. For the fifth consecutive year, diabetes has been the costliest traditional therapy class for payers. Industry research that looked at the recent trends in diabetes prescription data found that plans spent an average of $77.60 per member annually on diabetes medications in 2015, a 14% jump from 2014. The researchers noted that this increase was driven both by increases in use and high prices of treatments in the class. 
Insulin therapy remains a key component of diabetes treatment. More than 90 years of clinical data support its use, and it remains the most effective treatment to reduce glucose and hemoglobin A1c concentrations, even with the emergence of new drug classes for this disease state. However, insulin therapy is not without its drawbacks, such as its injectable delivery mode and its propensity to induce weight gain and hypoglycemia (Lancet Diabetes Endocrinol. 2015;3(8):638-652).
Effective Therapies at Debilitating Prices
Despite its longevity in the market and its proven effectiveness, a major challenge with insulin treatment has been the skyrocketing costs of these therapies in recent years. An analysis by Hua and colleagues, published in JAMA, showed that the cost of insulin more than tripled—from $231 to $736 a year per patient—between 2002 and 2013. The increase reflected rising prices for a milliliter of insulin; the mean price per milliliter of insulin increased by 197%, from $4.34 per milliliter to $12.92 per milliliter during the same time period.
According to a presentation by Irl B Hirsch, MD, of the University of Washington’s division of metabolism, endocrinology, and nutrition, given at the American Diabetes Association’s annual meeting in 2015, three of the top 6 drugs which have doubled in price in the last 5 years, are insulin products. Specifically, Dr Hirsh highlighted the 508% increase in the price of a vial of U-500 regular insulin over the past decade. Furthermore, Dr Hirsch disagrees with the notion that increases in use are to blame for the rising costs of insulin treatment, pointing to a decline in sales of human regular insulin between 2011 and 2014, from 5.8% to 3.9%.
Comparable New Insulin Therapies
New insulin therapies, such as insulin analogs including long-acting and short-acting insulin, offer comparable glucose control to older drugs. Compared with human synthetic and animal insulin for type 2 diabetes, short-acting insulin analogs may offer flexible dosing and convenience, and long-acting insulin analogs are associated with a lower incidence of nocturnal hypoglycemia. However, the prices for these drugs are 2 to 4 times greater than those of the older versions, according to research in JAMA.
In 2015, the US Food and Drug Administration approved four new insulin therapies: Toujeo (insulin glargine; Sanofi-aventis), Ryzodeg 70/30 (insulin aspart/insulin degludec; Novo Nordisk), Tresiba (insulin degludec; Novo Nordisk), and Basaglar (insulin glargine; Eli Lilly and Co). Basaglar is the first biosimilar to Sanofi-Aventis’ Lantus (insulin glargine). What is the cost of these recently approved insulin therapies? Tom Frank, PharmD, BCPS, director of research and education, University of Arkansas for Medical Sciences-Northeast, cited cost for two of these insulin therapies during a session on the costs of drugs in primary care at American Society of Health-System Pharmacists 2016 Summer Meetings & Exhibition. He reported that the cost of Novo Nordisk’s Tresiba is $426 for the U-100 concentration and $511 for the U-200 concentration. The cost of Sanofi-Aventis’ Toujeo is $322.06.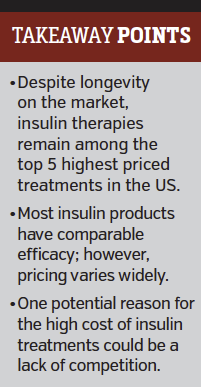
What Drives Prices Up?
According to available efficacy research, most approved insulin products are equally as effective and have similar safety profiles. So, what is driving up the cost of insulin therapies? One factor is that a lack of competition among insulin products has helped hold diabetes costs high. In 2014, Express Scripts made Lantus the preferred long-acting insulin on its National Preferred Formulary, in part because of its potential as the first long-acting insulin to face competition from a follow-on biologic. Currently, no generic insulin products are available; however, Basaglar is expected to launch in December 2016, which will offer financial relief to plans that prefer Lantus on their formularies.
Because stakeholders cannot forecast when the rising cost of insulin will slow, high prices will be an ongoing challenge for payers, health care providers, and patients.
“For many patients—especially those without insurance—the price of insulin is still too high to pay, and the consequences are disastrous for individual and systemic management of diabetes,” Jeremy A Greene, MD, PhD, and Kevin R Riggs, MD, MPH, both of the Johns Hopkins University School of Medicine, wrote in a commentary (N Engl J Med. 2015;372(12):1171-1175).













