Implementing Value-Based Care Through Clinically Integrated Organizations
 Can you explain what a clinically integrated organization (CIO) is and how one functions?
Can you explain what a clinically integrated organization (CIO) is and how one functions?
Defined, a CIO is an FTC-recognized model of physician group (joint) contracting based upon development of a robust quality improvement program with real accountability among otherwise independent physicians and hospitals or health systems. It integrates and rewards physician members around a common commitment to quality measures based on scientific evidence and cost improvement.
Alignment through a CIO with other physicians and organizations allows small practices to mitigate many of the challenges they’d face negotiating value-based contracts independently. For one, alignment means risk is shared across a more robust and medically diverse patient population. It also means physicians improve their contract bargaining power with payers.
In the end, CIOs provide the financial and operational bandwidth to succeed under a value-based model, leaving clinical care decisions where they belong: in the hands of patients and their doctors.
What factors influenced your organizations’ development of a clinically integrated care model?
In an effort to improve quality and contain costs, payers are moving away from fee-for-service contracting to a value-based system. For instance, Aetna, a commercial payer ranked in the Fortune 500, and other partner organizations predict that by 2020 as much as 75% of their business will be in value-based arrangements.
The Centers for Medicare and Medicaid Services (CMS), too, recently unveiled a plan to shift $362 billion of its non-managed-care budget to accountable care, bundled payments, and other payments that may offer rewards or penalties based on performance and cost savings.
With the move away from volume-of-service and a laser focus on value and quality, independent practitioners in small practices with limited staff support are sometimes ill-equipped to successfully broker meaningful contracts. Other prohibitive factors include limited patient populations, which can limit the ability of independent practitioners to effectively spread out risk.
Alignment through a clinically integrated model mitigates many of the challenges faced by small, independent practices. This model allays the financial, operational and technological limitations faced by small community practitioners through meaningful partnerships between and among private practices and a strong health system that’s willing to contribute the economic and human capital to support the network.
How is Phoenix Children’s clinically integrated care program unique?
Phoenix Children’s Care Network (PCCN), a dedicated pediatric CIO, is an alignment of close to 1000 community-based pediatricians, pediatric specialists, employed providers of Phoenix Children’s Hospital, and its various sites of service.
PCCN is rooted in a pediatric-dedicated quality improvement program that requires accountability among independent physicians and an aligned health system, incentivizing network providers for improving quality and controlling costs.
PCCN relies on data, integration, and alignment across the network to develop uniform standards for care delivery and evidence-based, preventative-focused clinical protocols for patients who fall within specific disease types, tenets of population health management.
PCCN includes more than half of all pediatricians and 80% of pediatric specialists in the Phoenix metropolitan area. It is a pediatric-dedicated CIO that positions its participating providers for success in the value-based contracting environment by facilitating improved continuity of care among participants and utilizing evidence-based clinical care guidelines developed by physicians. Participating providers and hospitals realize financial incentives for the delivery of high-quality, cost-effective care.
How do new value-based reimbursement models affect delivery of care?
Our model works because it unifies physician members and the hospital system around a shared commitment to quality improvement and cost efficiency. In PCCN’s ongoing development, we have moved from a volume-driven, fee-for-service model that creates inefficiencies and waste to a value-based system that rewards quality outcomes and cost control.
In fact, understanding the CIO premise that measurement is critical to performance, our physicians created 14 primary care and 34 specialist metrics encompassing safety, quality, and transparency outcomes. Provider reimbursement is now tied to these measures, holding us all to a high standard of quality outcomes and ensuring the right care is provided at the right place at the right time.
Why should organizations be interested in developing a clinically integrated care organization?
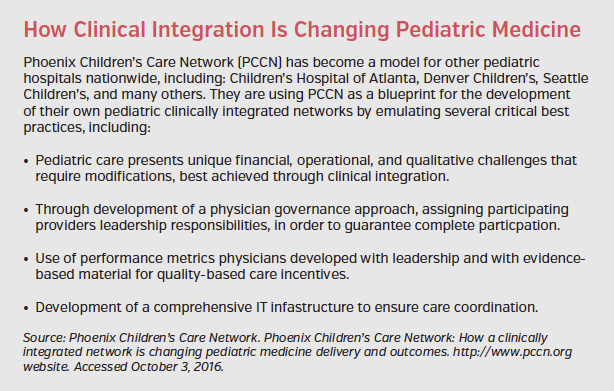
Accountable care practices present many benefits for pediatric medicine. However, pediatric care presents its own unique fiscal and operational challenges that require modifications in developing a CIO.
The success of the CIO depends on complete buy-in from physician and network partners. To that end, PCCN developed a physician governance approach, an especially important approach considering the majority of our network’s members are independent providers.
Incentives for quality and efficiency are based on metrics the physicians developed in concert with PCCN leadership. But most importantly, the CIO model effectively addresses three significant pain points of modern health care: rising costs, paltry reimbursements, and less-than-desirable outcomes.
Lastly, the need for a comprehensive and holistic IT infrastructure to coordinate communication, track data, facilitate integration, and manage cost and value is critical. As eHealth and telemedicine become imbedded in systems of care, IT will play an ever-increasing role in productivity and efficiency.
Your organization focuses solely on pediatric care, what made this model particularly beneficial when applied to this patient population?
In the same way that pediatric residencies and fellowships prepare physicians to treat pediatric injury and illness, our pediatric CIO has been built to achieve quality improvements specific to its patient population.
Unlike CMS’s 34 accountable care organization (ACO) quality metrics that are specifically geared toward adults, our performance measures are uniquely aligned with the population we serve. For instance, coronary artery disease and heart failure, two conditions measured by ACOs, are not common conditions among children. As such, we don’t measure quality for those conditions, instead focusing on metrics related to vaccinations, well visits, and asthma, all measurements that are germane to pediatric patients.
Have there been any outcomes associated with your organization’s clinically integrated care thus far?
Thus far the trajectory toward value-based contracting and effective management of the risk portfolio is extremely positive. Data indicators demonstrate PCCN’s efforts to improve care and control costs are working. Looking at outcomes from 2014, PCCN providers decreased the cost of care for the 50,000 patients it serves under Mercy Care, a not-for-profit health plan for Arizona’s Medicaid population. The care PCCN provided to these patients exceeded state quality standards in the following measures:
• Ensured babies younger than 15 months were seen at specific milestones.
• Children 3 to 6 years of age received their well exams and preventive services on time.
• The number of young adults 12 to 21 years of age attending their annual wellness visits increased, ensuring they enter adulthood healthy and with proper care.
• Ensured children aged 12 months to 11 years had appropriate access to a primary care pediatrician
• Ensured adolescents had appropriate access to a primary care pediatrician.
• Reduced asthma-related visits to the emergency room.
• Decreased overall emergency room utilization across entire patient population.
Is there anything else you would like to add regarding clinically integrated care, value-based care, or your organizations initiatives?
Value-based and population-health models are changing the complexion of health care. Fortified by the participation of a large number of physicians and mature health systems focused on improving care and managing costs, CIOs are equally appealing to payers actively developing value-based contracts.
As CIOs gain popularity across the country, more payers and large employers are seeking alignment with clinically integrated networks to curb costs and offer more competitive, complete health coverage.
The equation is based on an incentive framework: compensation depends on the implementation of meaningful performance measures and the achievement of corresponding outcomes, not on procedures and volume. As the health care marketplace continues to adjust rapidly, requiring leaders to craft and implement adroit strategic initiatives, efforts such as PCCN provide a winning and repeatable formula for ensuring the finest health care for patients.










