ADVERTISEMENT
Exondys 51: Controversy in the Wake of an Unprecedented FDA Approval
 Shortly after the unprecedented approval of Exondys 51 (eteplirsen; Sarepta Therapeutics), the first drug ever approved to treat Duchenne muscular dystrophy (DMD), Anthem Inc announced it would not cover the drug under its insurance plans, due to a lack of efficacy evidence presented during the drug’s FDA approval process.
Shortly after the unprecedented approval of Exondys 51 (eteplirsen; Sarepta Therapeutics), the first drug ever approved to treat Duchenne muscular dystrophy (DMD), Anthem Inc announced it would not cover the drug under its insurance plans, due to a lack of efficacy evidence presented during the drug’s FDA approval process.
Experts say Anthem’s recent decision not to cover Exondys 51 was an outlier—not because of the drug’s still uncertain efficacy but because of the small patient population it will impact.
“Anthem is kind of stepping out here on something that’s really unlikely to cost them a lot of money,” Jim Lee, MS, vice president at Altarum Institute, a nonprofit health systems research and consulting organization, said in an interview.
However, almost immediately following Anthem’s announcement, Humana announced that they would only cover the drug under limited conditions. Humana’s conditional coverage plan states that it will cover 6 months of the drug, followed by another 6 months only if patients continue to be ambulatory.
The Food and Drug Administration (FDA) approved Exondys 51 in September through the accelerated approval pathway, but not before it was met with some controversy.
For instance, this spring, the Peripheral Central Nervous System Drugs Advisory Committee of the FDA recommended against approving the drug as a DMD treatment and several studies into its use have failed to meet their primary endpoints. While at the same time, Ronald Farkas, MD, PhD, supervisor of the FDA’s clinical review of eteplirsen, resigned after expressing concerns of the lack of efficacy found during clinical trials.
However, the FDA ultimately did approve the drug using a surrogate endpoint; however, as part of their decision, they are also requiring Sarpeta Therapeutics, the company who makes Exondys 51, to conduct a clinical trial to establish the drug’s clinical benefit after approval.
In the weeks that have followed its approval, payers response to the drug’s approval has been mixed.
For instance, Anthem issued a medical policy announcing it wouldn’t cover Exondys 51 because they believe it’s “investigational and not medically necessary.”
However, Cigna and United Healthcare have both said they will cover the medication.
While Cigna plans to cover the drug for those patients who have a confirmed mutation of a specific section of the DMD gene, they also acknowledge that because it received accelerated approval by the FDA, a definitive clinical benefit of the drug has not yet been established.
“We will continue to follow the clinical trials of Exondys 51 to ensure that this new drug is delivering value to Cigna’s customers and clients for the money they are spending,” Karen Eldred of Cigna public relations told First Report Managed Care.
United Healthcare has said it will cover Exondys 51 under its medical benefit, with prior authorization.
Experts say they understand why Anthem made the decision not to cover a drug without established clinical efficacy, but say what makes the decision interesting is that payers have typically covered orphan drugs due to the low number of members they affect and the lack of other therapeutic options.
“In the past, the payers typically covered rare diseases,” Eileen Pincay, BS, RPh, senior pharmacy consultant for The Segal Group’s national pharmacy benefits practice, said in an interview.
According to the FDA, DMD occurs in about 1 out of 3600 male infants across the world and rarely affects females. Out of this population, Exondys 51 is used to treat specific DMD patients who have a mutation of the dystropin gene amenable to exon 51 skipping, which occurs in about 13% of the patient population with DMD.
“This is such a small population,” Mr Lee said. “I think many payers are going to look at this and say, is it worth the down side that Anthem may be taking here by not approving this, if they look through and see they only have 4, 5, or 6 people covered?”
The Rationale for Approval
DMD has been described by the FDA as a rare genetic disorder that causes progressive muscle deterioration and weakness in patients.
“If a patient has this disease, they typically start at a young age, so maybe 5 years of age and by the time they are teens they are in wheelchairs. So, it is very devastating,” Ms Pincay said. “This disease can actually progress, it can cause heart, lung disorder, and eventually death.”
There are currently no DMD approved drugs on the market and Ms Pincay says patients are typically prescribed drugs like prednisone, which can slow muscle deterioration but can also cause weight gain and weaken the bones causing fractures over time.
The FDA ultimately decided to grant accelerated approval to Exondys 51 based on an increase in dystrophin seen in the skeletal muscle of some patients treated with Exondys 51, a finding that served as the surrogate endpoint.
However, whether that increase translates to any clinical benefit, including improved motor function is yet to be seen.
According to Susan Winckler, a chief risk management officer with Leavitt Partners, while some were surprised Exondys 51 received approval from the FDA, others were not.
“Congress told the FDA to pay attention and start to do patient-focused drug development and pay attention to and use surrogate endpoints, and so the FDA review process is undergoing some revision as society also says we also have access to more information about making decisions about how to use these products,” Ms Winckler said, who formerly served as chief of staff for the FDA.
She believes some payers could reach different conclusions about the approval of Exondys 51 because they are answering a different question than the one that was posed to the FDA.
While the FDA was looking at whether the drug is safe and effective, payers themselves are deciding whether this is an area they want to spend their resources.
“So, FDA’s review is of the package in front of them and there’s some consideration of that broader environment, but the payer’s consideration is about the broader environment and the available treatment options, drug and nondrug,” she said.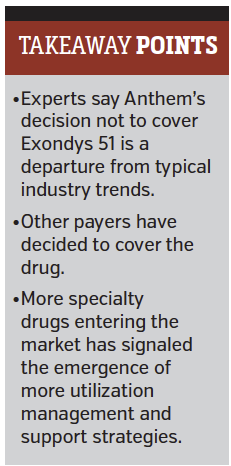
Ms Winckler explained that some payers’ decisions not to cover the drug are likely less about its approval with a surrogate endpoint and more about the FDA’s instruction that a confirmatory clinical trial must be conducted after approval.
“Perhaps it’s creating a bit more gray space between investigational and approved and so I think it also gives a little more rationale to payers who want to say, we want to see the results of the ongoing study,” she said.
Experts agree that once the confirmatory clinical trial has concluded, more will be known about the future of Exondys 51.
Ms Pincay said if the study shows a clinical benefit, it’s likely Anthem will decide to offer coverage. If it doesn’t, other plans may choose to stop covering it.
Impact for Managed Care
Exondys 51 is just one example of many, new orphan drugs hitting the market.
A recent study from the Segal Group estimated that the projected specialty drug and biotech trend rate for 2017 will be 18.7%. In addition, while usually less than 1% of all medications are specialty drugs, the survey found that those drugs are estimated to represent 35% of total projected prescription drug costs in 2017.
Many of these drugs often carry a high price tag. For example, Exondys 51 is estimated to cost about $300,000 a year.
Ms Pincay acknowledged that the specialty drug trend continues to rise; however, she said despite the recent example with Anthem, she thinks most payers will continue to cover specialty and orphan drugs entering the market.
“I foresee payers not putting much barriers on it because of the fact that it’s for a small population,” she said.
Instead, experts say they’ve seen more evidence that payers will put more steps and policies in place to make sure specialty drugs are being given to the right patients.
“We’re seeing much more evidence that they are much more careful about prior authorization,” Mr Lee explained, adding that payers are now more frequently requesting evidence from an approved lab to ensure the patient will benefit from the therapy.
Mr Lee also said he could see a drug like Exondys 51 being used in pay-for-success or pay-for-performance type contract.
With a greater emergence of precision medicine, Ms Winckler said she believes it will be important for payers to correctly align their precision medicine to protect the investment they have made in therapy options.
“You invest in the diagnostic test to make sure it’s tied to the new medication, and then if that new medication is going to be invested in, do we make sure that we have the right resources to support the patient in making the best use of that medication?” she said.
As payers and managed care organizations make decisions about where they want to invest their resources, Ms Pincay said she recommends that her clients first look at their own patient population.
“For my clients, I would recommend first trying to see what the member impact is, if any,” she said. “It could be very, very small and I recommend putting controls in place, looking at opportunities for utilization management, especially in the top therapeutic categories.”
Each payer’s response may differ to the emerging world of specialty pharmaceuticals, but experts say all payers will be looking for strategies and approaches to limit costs and effectively treat their patient populations.





















