Employing Managed Care to Avert a Diabetes Epidemic
 The US health care system is facing an epidemic that if not slowed now will continue to take an extraordinary toll on the quality of people’s lives and exact an equally extraordinary burden on society in terms of morbidity and cost.
The US health care system is facing an epidemic that if not slowed now will continue to take an extraordinary toll on the quality of people’s lives and exact an equally extraordinary burden on society in terms of morbidity and cost.
That epidemic is diabetes. Currently, 1 in 10 adults in the United States have diabetes—a number predicted to grow sharply over the next decades to 1 in 3 by 2050 if the current trend continues.
In a recent interview with First Report Managed Care, Albert Tzeel, MD, a regional medical director at Humana, summed up the possibility of a diabetes epidemic by drawing attention to the present state of diabetes in America.
“If one defines an ‘epidemic’ as a widespread occurrence for a given event, I would say that type 2 diabetes has already reached epidemic proportions. With the almost 30 million Americans (nearly 10%) who suffer from diabetes right now,” he said. “I am concerned and I think that, from a public health standpoint, we all should be.”
Furthermore, diabetes itself is not the entirety of the problem. Most patients with diabetes have a range of comorbidities that require long-term treatment and management, and contribute significantly to poor health outcomes and the substantial cost burden. According to Dr Tzeel, about 30% of Americans have prediabetes—defined as medical conditions heightening their risk of developing type 2 diabetes within 10 years to 70%.
Estimates by the Centers for Disease Control and Prevention (CDC) place the total costs of diabetes at $174 billion annually, $116 billion of which is for direct medical costs. In 2016 alone, the CDC estimated that Medicare spent $42 billion more for beneficiaries over age 65 with diabetes than it will spend on beneficiaries without diabetes.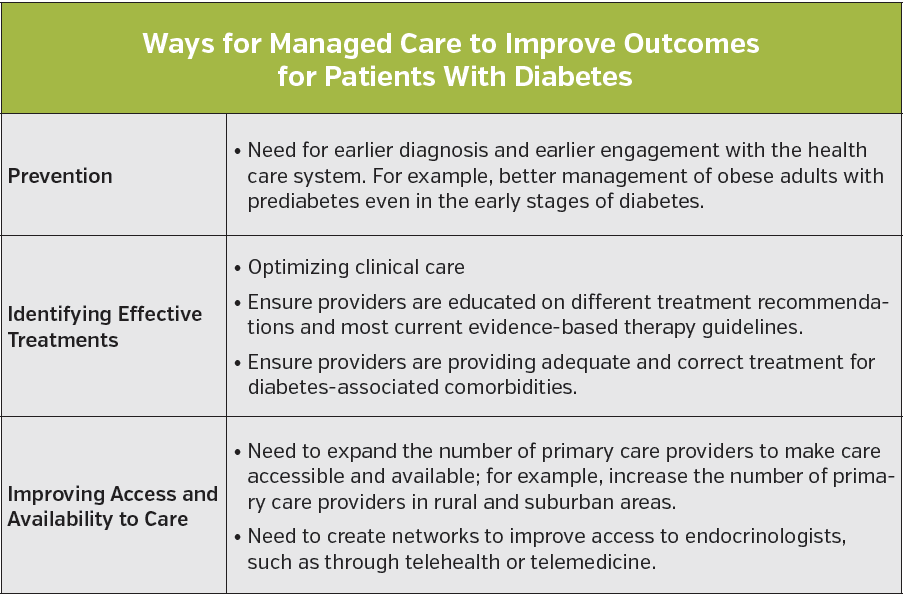
Underlying the already current burden of this disease is its impending progression. “We are in the midst of a tsunami warning,” Thomas Morrow, MD, chief medical officer of Next IT and a managed care consultant, said in an interview.
Dr Morrow highlighted that the real burden of diabetes will be felt when the millions of patients currently diagnosed or undiagnosed with pre-diabetes develop full-blown diabetes if nothing is done to prevent it.
Currently, he said, 1 in 4 adults in the United States have prediabetes. Although he said that while the pancreases in these patients are already failing, providers in the United States on the whole are failing to aggressively treat and thus missing an opportunity to prevent diabetes in about 50% to 77% of them.
Clearly, the current and projected burden of diabetes is pressing and will continue to place an enormous burden on the US health care system unless steps are taken to meaningfully address the problem. To date, some steps are being made such as provisions in the Affordable Care Act that mandate coverage for patients with prediabetes and a 2016 program launched by the Centers for Medicare and Medicaid (CMS) called the Diabetes Prevention Program (DPP) to manage and prevent prediabetes.
Improving Outcomes and Reducing Costs
John A Johnson, MD, MBA, FACP, senior medical director of WellCare in Atlanta, emphasized three issues that are essential for managed care to address in improving the health of patients with diabetes as well as cutting costs; including prevention, identifying effective treatments, and improving access to care (Table).
Along with prevention, Dr Johnson said that managed care needs to ensure that providers are offering patients with diabetes the best clinical care by treating both their diabetes as well as the many comorbidities that accompany the disease. Likening the treatment of diabetes in the United States to making chili, he emphasized that everyone approaches treatment with their own recipe comprised of different oral antidiabetic medications and different types of insulin.
“We need to connect physicians and providers who treat patients with diabetes and prediabetes to the most current evidence-based therapy to ensure that there is no medical inertia,” he said, and added that medical inertia is when physicians fail to counsel their patients toward a goal in their treatment and instead simply refill their patients’ medications without talking about lifestyle modifications that could improve their disease.
At WellCare, he makes sure that all providers in the network have access to clinical practice guidelines from the American Diabetes Association or American Association of Clinical Endocrinologists to provide them with evidence-based suggestions for managing their patients with diabetes.
 Along with providing the best clinical care, Dr Johnson stressed that managed care needs to make sure that such care is available and accessible to all patients who need it.
Along with providing the best clinical care, Dr Johnson stressed that managed care needs to make sure that such care is available and accessible to all patients who need it.
“We have to make sure that there are enough access points for patients to be connected to the health care system,” he said, highlighting the need to expand primary care providers into rural and suburban areas.
In addition, he emphasized the need for managed care to develop networks to ensure that primary care providers can work with endocrinologists to tailor the best care for their patients.
“Managed care plans need to become more innovative and they need to leverage technology to connect patients to care,” he said, suggesting the use of technologies such as telehealth and telemedicine to connect primary care providers and patients to endocrinologists.
“This will give primary care providers more comfort in managing diabetes in their office if they have remote access to endocrinologists,” he added.
Prevention as the primary focus
Of all the issues that managed care can address to reduce the burden of diabetes, according to Dr Morrow, the most important is to focus on prevention.
“Diabetes is really just a symptom of a greater problem, and that is our nutrition and exercise habits in the United States,” he said, adding that underlying the diabetes epidemic for people with the full-blown disease as well as for the tens of millions with prediabetes is another epidemic—obesity.
“Obesity is the largest risk factor for diabetes,” he said, emphasizing the need for providers and the health care system as a whole to educate people on the need to lose weight and exercise more.
He stressed that people with normal weight who are at risk for prediabetes also need to be educated on the need for regular exercise and, importantly, on eating a nutritious diet.
“Eating a balanced, high plant-based diet is rare in the United States, where the two most commonly eaten plants are potatoes in the form of French fries and tomatoes in the form of ketchup,” he said.
Dr Johnson also highlighted the need to educate managed care providers on the risk factors for diabetes among which is being overweight or obese. He noted that this can be difficult because providers have to attack diabetes on multiple fronts.
“In managed care, once you get a handle on the diabetic population and then move over to the prediabetic population, simultaneously you have to handle the overweight and obese populations,” he said.
Specific Initiatives Underway
Several initiatives are underway to help providers identify patients at risk of diabetes and to help with prevention. Among these is the DPP by CMS to manage and prevent the onset of type 2 diabetes in beneficiaries diagnosed with prediabetes. Scheduled to begin on January 1, 2018, the program is a 12-month intervention offered in community and health care settings in which eligible beneficiaries work with coaches to learn and adopt lifelong dietary changes, increased physical activity, and behavior changes for weight control (diet, lifestyle issues, and moderate physical activity).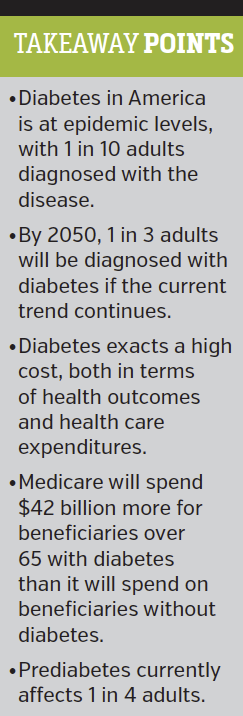
Initiatives underway through managed care include case and disease management programs, according to Dr Johnson. These programs offer field-based, in-home support, or support by telephone to members with diabetes who are having lifestyle or socioeconomic challenges. Members are identified and selected for these programs via direct referrals as well as proprietary algorithms based on pharmacy and medical claims data.
To help members who are covered by Medicare or Medicaid, Dr Johnson said that WellCare has an advocacy program to connect members to community resources to help them make behavioral changes related to diet and lifestyle needs.
Another way to promote better engagement from providers to help prevent diabetes is to contract with providers through value-based purchasing agreements, said Dr Johnson.
“We’ve been moving a lot of our members with diabetes under providers associated with patient-centered homes or through value-based purchasing agreement,” he said.
Dr. Morrow emphasized the need for managed care providers to become familiar with nontraditional ways to access prevention programs for people with prediabetes, including online networks such as Solera Health and Equity Healthcare.
Such networks provide a way to scale-up prevention programs by offering a digital platform and mobile technology to deliver programs. For example, Solera Health has created a virtual marketplace for a variety of diabetes prevention vendors ranging from totally digital approaches to digitally-integrated human coaches via telephone and the internet.
According to Dr Morrow, Solera Health was the first marketplace for prediabetes programs and has contracts with numerous managed care companies. Equity Healthcare is also a marketplace that plans to include a wide variety of medical services from total joint replacements to radiology procedures as well as prevention programs on their site, said Dr Morrow. Equity Healthcare plans to go live by second quarter 2017.
Message of Managed Care Providers
Both Dr Johnson and Dr Morrow emphasized the need for managed care providers to pay close attention to the management and prevention of diabetes.
“Make sure your members with obesity, pre-diabetes, and diabetes are all connected to an appropriate level of care so they receive preventive services,” Dr. Johnson advised managed care professionals.
Dr Johnson also emphasized the need for a model for diabetes care and prevention that is cost-effective and leads to more improved quality outcomes.
According to Dr Tzeel, big data could play a huge part in reducing the potential burden of a diabetes epidemic.
“A key area where managed care organizations can play an important role in averting a health care resource disaster is through the use of analytics,” Dr Tzeel said in an interview. “We have a tremendous amount of data that we capture from various sources: claims data, lab data, demographic data, and—in cases where we can perform health information exchange with our providers—certain electronic medical records data. The ability for us to mine that data for the gold nuggets of information and knowledge that it can provide to help us see patterns that might otherwise not be seen is incredible.”
For Dr Morrow, the need to improve diabetes care and, most importantly, prevention is imperative for the financial survival of the health care system as we know it.
“Although every health plan in the United States has a diabetes program, few of these plans actually have a fully functional diabetes prevention program,” he said. “We need to pay a lot of attention to this or literally it will bankrupt our country. We cannot afford this disease.”












