Drawing Battle Lines: Expansion of Nurse Practitioner Authority Within the VA
 A recently proposed rule by the Department of Veterans Affairs (VA) to expand full practice authority to advanced practice registered nurses (APRNs) garnered more than 160,000 public comments, emphasizing the tension between groups on both sides of this issue.
A recently proposed rule by the Department of Veterans Affairs (VA) to expand full practice authority to advanced practice registered nurses (APRNs) garnered more than 160,000 public comments, emphasizing the tension between groups on both sides of this issue.
If the proposed rule is enacted into law, all APRNs will be granted full practice authority throughout the VA system nationwide. Currently, 21 states and the District of Columbia already permit full practice authority to APRNs; therefore, the proposed rule would extend this privilege to all APRNs in states that don’t currently permit this.
Considerable pushback has come from a number of medical organizations. Opposition has been based on concerns ranging from encroachment on state practice authority to undermining physician-led, team-based care models. Physicians’ associations also expressed concerns over the potential harm the proposed rule could have on the quality and safety of care given to veterans.
Public comment closed on July 25, 2016, and no timeline has been given as to when the final rule will be made public.
Understanding the Rule
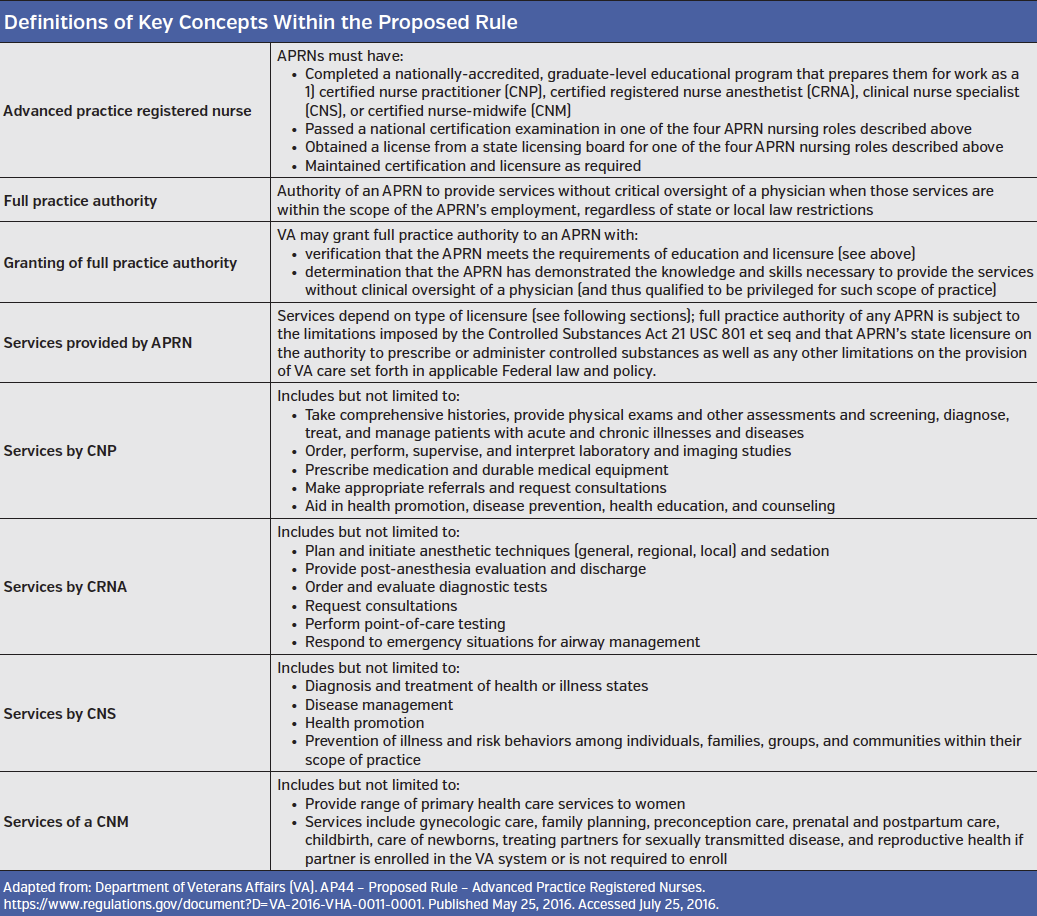
Published May 25, 2016, in the Federal Register, the rule, titled “Advanced Practice Registered Nurses,” proposes “to amend its medical regulations to permit full practice authority of all VA APRNs when they are acting within the scope of their VA employment.”
According to Penny Jensen, DNP, APRN, FNP, FAAN, FAANP, of the National APRN Health Policy Liaison for the Office of Nursing Services at the VA, the agency has been working on making changes to nursing policy since 2009.
“The proposed rule permits the VA to use its health care resources more effectively and in a manner that is consistent with the non-VA health care sector, while maintaining the patient-centered, safe, high-quality health care that veterans receive from the VA,” she said.
Dr Jensen, who has practiced for the past 18 years as a nurse practitioner at Outpatient Primary Care Clinics in the Salt Lake VA Health Care System and is currently an assistant professor at the University of Utah College of Nursing, explained that each state has its own standard regarding the role of APRNs in the VA system.
Emphasizing that the VA is an integrated federal health care system, Dr Jensen said that the proposed policy to expand APRN authority parallels the current policy in the Department of Defense (DOD).
“Service members transitioning from DOD to the VA should be able to receive the same health care services from APRNs in both systems,” Dr Jensen said, adding that many VA medical centers are already successfully using both nurse practitioners and certified registered nurse anesthetists to the full extent of their education and training.
The Underlying Need
One big driver of the proposed rule is to help increase the capacity of the VA to provide timely health care to veterans. According to Cindy Cook, DNP, FNP-C, FAANP, president of American Association of Nurse Practitioners (AANP), delay of care to veterans is the major reason for the proposed rule, and using nurse practitioners to the full scope of their education and training would decrease wait time for veterans.
“Right now there are over one-half million veterans waiting 30 days or longer to receive care at a VA facility,” she said. “What this proposal would do is increase the number of appointments across the nation and hopefully decrease the wait times for our veterans.”
Supporting this approach to decreasing wait times and increasing faster and better access to care is the recognition that limitations on the scope of practice for nurses has both undermined their full ability to provide care and limited the ability of the health care system overall to provide quality care.
As stated in the proposed rule and underscored by Dr Jensen, the rule is consistent with a 2010 report by the Institute of Medicine (IOM) of the National Academy of Sciences called “The Future of Nursing: Leading Change Advancing Health” that recommended allowing nurses to practice to the full extent of their education and training.
Expressing concerns that the abilities of nurses to provide and improve general and advanced health care are undermined by restrictions on the scope of their practice, Dr Jensen emphasized that the IOM report also provided “expert advice based on evidence, suggesting that access to quality care can be greatly expanded by increasing the use of… APRNs in primary, chronic, and transitional care.”
Furthermore, Dr Jensen cited the AANP’s Quality of Nurse Practitioner Practice Position paper, which shows that “the body of literature supports the position that nurse practitioners (NPs) provide care that is safe, effective, patient-centered, timely, efficient, equitable, and evidence-based” and that “NP care is comparable in quality to that of their physician colleagues.”
Opposing Forces
Among the number of organizations opposed to the proposed rule are the American Medical Association (AMA), the American Academy of Family Physicians (AAFP), and the American Society of Anesthesiologists (ASA).
“We feel this proposal will significantly undermine the delivery of care within the VA,” Stephen R Permut, MD, JD, board chair of the American Medical Association, said in a statement. Specifically, he stated, “Providing physician-led, patient-centered, team-based patient care is the best approach to improving quality of care for our country’s veterans.”
Robert L Wergin, MD, board chair of the AAFP, also emphasized the importance of physician-led, team-based health care delivery in a letter to the VA.
“This proposal would alter the consistent standards of care for veterans over non-veterans in the states, further fragment the health care system, and dismantle physician-led team-based health care models,” he wrote in the letter.
Daniel J Cole, MD, president of the ASA, also stressed the need to keep a physician-led, team-based model of care in place.
“From our perspective, the best solution is to leave anesthesia as it is,” he said, which, he added, is “very high-quality team-based care where both physicians and nurse anesthetists practice together.”
Emphasizing the high value and competency of nurse anesthetists as members of the anesthesia care team, Dr Cole also stated that “potentially removing the physician from the high-stakes decisions that are made in a matter of seconds and occur frequently throughout intraoperative care would lower the standard of care and put veterans’ lives at risk.”
Although Dr Cole said he understood the premise of the proposed rule to address a shortage of physicians in primary care in the VA system, he added that the premise of the rule is not relevant to anesthesiology because there is currently no shortage of anesthesiologists. A study published in 2015, by Carrie M Farmer, PhD, a senior policy researcher at Rand Corporation, and colleagues, did not list physician anesthesiologists among the 12 provider types in which shortages within the VA were found. However, according to
Dr Farmer and colleagues, their research was based on a small sample of interviews, so the results cannot reliably be used to identify systematic shortages. Dr Cole also stated that the ASA did its own assessment and found little indication of a shortage of physician anesthesiologists working within the VA system.
As such, he said the proposed rule to extend full practice authority to include certified nurse anesthetists is “a solution in search of a problem, and a solution that will cause problems with anesthesia care.”
Dr Cole added that, at the very least, inclusion of certified nurse anesthetists in the proposed rule should be carved out.
 Addressing Veterans’ Complex Needs
Addressing Veterans’ Complex Needs
With the public comment period now closed, the VA will begin its work to finalize the rule, taking into consideration more than 160,000 comments both in favor and against extending full authority practice to APRNS.
For those in favor, the hope is that APRNs will be able to practice at the full scope of their skills, education, and training.
Dr Cook emphasized the need for full collaboration among health care providers to meet the needs of patients. Citing her 12 years of experience working as a primary care provider in a military setting, Dr Cook said, “If you trained a soldier to do 10 things you would want them to do all 10 things and not just three. NPs, along with every other health care provider, collaborate with other physicians each and every day to make sure the patients’ needs are met.”
She added, “It takes a variety of health care professionals from different disciplines to meet the complex needs of our veterans who require some chronic and complex care.”
Those against the rule cite the compromise in care and the potential harm to veterans if a physician-led, team-based model of care is altered.
In a statement to the VA, Dr Wergin concisely expressed the consensus among those opposed to granting full practice authority to APRNs.
“Physicians and nurses occupy interdependent roles in the delivery of quality, comprehensive health care,” he said. “Physicians offer an unmatched service to patients and, without their skills, patients’ safety would be at risk.”













