Cessation of Treatment May Be Possible for Patients With Chronic Myeloid Leukemia
 According to two studies presented at the 2016 ASH Annual Meeting and Exposition, patients with stable chronic myeloid leukemia (CML) may be able to safely cease or reduce treatment with tyrosine kinase inhibitors (TKIs) in order to avoid side effects and treatment costs.
According to two studies presented at the 2016 ASH Annual Meeting and Exposition, patients with stable chronic myeloid leukemia (CML) may be able to safely cease or reduce treatment with tyrosine kinase inhibitors (TKIs) in order to avoid side effects and treatment costs.
TKIs such as Tosigna (Nilotinib; Novartis), imatinib, and dasatinib effectively treat patients with CML; however, the side effects and financial costs of treatment can be a burden. While guidelines recommend continuing TKI treatment even after achieving remission, researchers have recently questioned if patients who have successfully controlled their CML can safety reduce or cease treatment after stabilizing. Side effects often include cramps, fluid retention, excess fluid around the lungs, skin rashes, nausea, vomiting, diarrhea, damage to the heart, and fatigue. Women taking TKIs are also advised not to plan pregnancies, as there is a high risk for fetal birth defects.
Complete Cessation Safe?
“Many patients struggle between the decision to stop TKI use because of its side effects and the fear of remission,” Francois-Xavier Mahon, MD, PhD, a lead study author and a director at the Bergonie Cancer Center of the University of Bordeaux in France, said in a press release. “Because of the high number of patients included in [our] study, we think the results could help to inform future guideline recommendations for TKI use.”
Dr Mahon conducted one of the largest ever trials on the safety of ceasing TKI treatment between 2012 and 2014. They analyzed 821 CML patients without prior TKI failure treated with Tosigna, imatinib, or dasatinib. The researchers observed study participants who reached deep molecular responses to TKIs and stopped treatment. They defined molecular reoccurrence as the loss of the major molecular response at any point.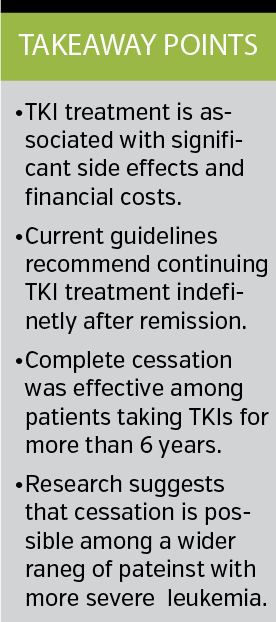
The researchers found that patients who received TKIs for more than 5.8 years were significantly less likely to relapse within the first 6 months of cessation. Molecular recurrence-free survival was 62% at 6 months after cessation, 56% at 1 year, and 52% at 2 years. According to the study results, 348 patients lost major molecular response and 5 patients died in remission during the study period.
Furthermore, the researchers found that most patients regained deep molecular responses with no progression to advanced disease phase found among study participants.
Dr Mahon and colleagues noted that cost savings for reduced treatment regimens amounted to an estimated €27.85 million.
Dr Mahon and colleagues’ study was funded by the by European Leukemia Net and was partially funded by the French National Institute of Cancer.
A Wider Range of Patients
A second study presented at the 2016 ASH Annual Meeting and Exposition found that a wider range of CML patients may be able to safely reduce their TKI dosage by half than previously thought.
Previous trials, such as the one above, often focused on reducing TKI therapy among patients who are essentially clear of leukemia. However, this study also included patients with a stable MR3 remission level. According to the press release, the researchers described this remission status as “good, but not perfect.”
The researchers noted that although some limited anecdotal evidence exists for the cessation of TKIs among stable MR3 patients, such as cessation during pregnancy, the stopping trial has not been formally performed among this patient population.
In order to determine safety among this patient population, the researchers studied 174 patients receiving Tosigna, imatinib, or dasatinib. The researchers initially decreased TKI therapy by half for 1 year and then commenced complete cessation.
Study results showed that 93% of study participants showed no evidence of CML reoccurrence during the 1-year period after cutting their doses in half. Among the entire study population, only 12 patients experienced CML reoccurrence and all regained remission after continuing normal TKI dosage levels.
The researchers also found that many patients experienced a significant decrease in TKI-related side effects. However, they noted that 21% of patients reported 53 new mild and transient musculoskeletal symptoms.
“Taken together, these findings might indicate that some patients are being unnecessarily over-treated,” Mhairi Copland, MD, PhD, lead researcher and professor of translational hematology at the Institute of Cancer Sciences at the University of Glasgow in the United Kingdom, said in the press release. “The other important implication is that patients do not have to have extremely low levels of leukemia on very sensitive tests in order to safely try reducing their TKI dose.”
The researchers also noted that any benefits associated with cessation, such as reducing adverse effects, are likely to become apparent within the first 3 months.
This study was funded by the University of Newcastle and the UK-based the blood cancer charity Bloodwise. —David Costill














