Advances in HIV Treatment: Better Control For Higher Prices
Breakthroughs in Infectious Diseases is a 3-part series aimed at identifying the challenges managed care professionals face when making infectious disease related decisions and the latest breakthroughs that can help solve those issues. The series will provide an in-depth look at the most pressing treatment developments in HCV, HIV, and other infectious diseases.
The continual development of new drug regimens to treat HIV infection has transformed this once fatal disease into one that is chronic for many patients. Many patients now live with stable disease maintained by increasingly simpler ways to administer treatment by lowering the pill burden and dosing frequency and by treatment regimens that are less toxic and better tolerated, according to research in Clinical Infectious Diseases. Over the past decade, the arrival of once-daily, single-tablet regimens has provided the latest drug regimens to ease the burden of treatment administration for patients.
As with many new therapies, however, these new drug regimens can carry a high price tag, one that places a burden on patients, payers, and society as a whole. The monthly average wholesale price for these new regimens range from $2462 to $2949. As such, defining the best use for these therapies is important to ensure that patients are receiving the best care in the most cost-effective way.
In order to better understand this burden, First Report Managed Care looked into how these newer drug regimens have affected outcomes for persons living with HIV, the cost of these regimens, and issues important to consider when weighing the cost of these regimens, particularly the issue of switching therapies.
The Outcomes Data
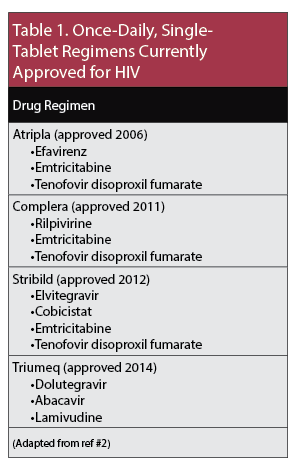 The US Department of Health and Human Services (HHS) currently recommend the use of once-daily, single-tablet antiretroviral treatment regimens as initial therapy for treatment-naïve patients. Table 1 lists the four regimens currently approved for use. [A fifth regimen combining cobicistat, emtricitabine, and tenofovir alafenamide was submitted for new drug application for HIV treatment in September 2017 and pending review.]
The US Department of Health and Human Services (HHS) currently recommend the use of once-daily, single-tablet antiretroviral treatment regimens as initial therapy for treatment-naïve patients. Table 1 lists the four regimens currently approved for use. [A fifth regimen combining cobicistat, emtricitabine, and tenofovir alafenamide was submitted for new drug application for HIV treatment in September 2017 and pending review.]
Retrospective data show that patients taking these regimens are more likely to achieve 95% adherence than patients taking two or more pills a day. Achieving at least 95% adherence is important as data show that adherence rates that are lower than this are linked to virological failure and development of antiretroviral resistance.
These data also show that the rate of hospital admissions is significantly reduced in patients taking once-daily, single-tablet regimens compared to multidrug regimens, with one study showing a 26.8% reduction and another study showing a 23% reduction.
Lowering the pill burden has emerged as a key factor effecting outcomes in patients with HIV. This was shown in a 2014 meta-analysis conducted by Jean B Nachega, MD, PhD, MPH, and colleagues, to investigate the effect of pill burden and dosing frequency (once-daily vs twice-daily dosing) on adherence to antiretroviral therapy (ART) and virological outcomes. The meta-analysis, which included 19 randomized controlled trials and total of 6312 patients, found that a higher pill burden was associated with lower virological suppression regardless of dosing frequency. Dosing frequency was found to have only a modest effect on adherence, with adherence only slightly increased in patients taking once-daily regimens, and no effect on virological suppression.
“Our results suggest that pill burden should be a consideration in the selection of an antiretroviral regimen, independent of dosing frequency,” the researchers concluded.
Although none of the studies included in the meta-analysis directly evaluated the effect of a fixed-dose, single-tablet regimen, the investigators suggest that single-tablet regimens may be helpful in some patients given the finding of a significant negative association between pill burden and viological suppression.
“The nonlinear correlation between pill burden and adherence or virological suppression suggests that, while ART desimplification from once-daily single-tablet regimens to once-daily multitablet regimens may have adverse effects on virological outcomes, separating out single-tablet regimens and/or fixed-dose combinations into their constituents is not likely to have a major detrimental impact on virological outcomes (provided that the overall pill burden does not increase dramatically),” conclude the investigators.
However, they cautioned that more research is needed on the effect of switching patients, particularly those that are virologically suppressed at baseline.
Article continues on page 2
Cost of Newer HIV Regimens
To gain a better understanding of recent treatment patterns and cost of HIV in the United States, a recent study looked at health care costs of HIV patients by treatment line (first, second, or third) and CD4 cell count. Using data compiled from commercially insured patients in 12 health plans in the United States, the study included the cost of newly treated patients between January 2007 and December 2011 who had at least one treatment line lasting 90 days or more.
Overall, more than 20% of patients switched their initial treatment regimen within 2 years. Table 2 lists the costs of treatment by treatment line.
The study found that, after adjusting for covariates, second-line treatment was significantly more expensive than first-line treatment (24%; P < .001) as was third-line treatment (41%; P = .006).
When looking at CD4 cell counts, the study found that inpatient admissions became an increasing driver of cost in patients with lower CD4 cell counts. For patients with higher CD4 cell counts, the major driver of cost was the cost of antiretrovirals (64%). Table 3 lists costs by CD4 cell counts.
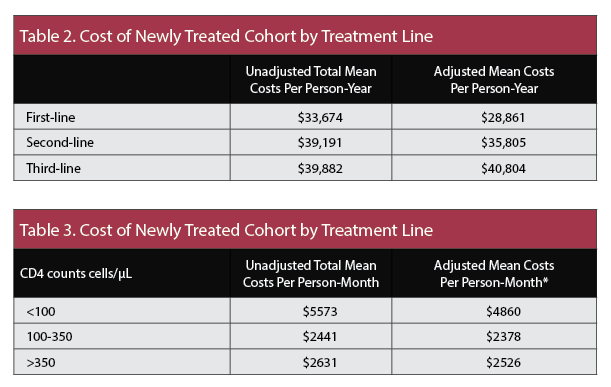
The study found that patients with CD4 cell counts < 100 cells/µL had significantly higher costs per person-month by 92% compared to patients with CD4 cell counts of <350 cells/µL (P < .001).
The results of this study showed that “during the years 2007 through 2011, US patients receiving first-line treatment had significantly lower total health care costs than patients receiving second-line or third-line therapies.”
“This indicates,” they continue, “that further investment to develop additional treatment regimens to suppress viral replication and preserve patients’ CD4 cells through multiple lines of treatment are fundamental to long-term HIV disease management, and reduction of the economic burden of advanced HIV disease.”
A more recent study published in The Journal of Managed Care Pharmacy also found that patients who switch treatments incur a higher cost. In the study, investigators looked at the effect on health care utilization and cost of first-line regimen switching in HIV patients with stable disease.
Using claims data from different health care providers in the United States on 6983 adult patients with HIV who initiated ART between 2007 and 2013, investigators found that, after adjusting for type of ART, demographic data, comorbidities, and baseline total health care costs, follow up health care costs were 8.9% higher among patients who switched treatment compared to those who remained on their initial treatment.
The study found that the increased cost incurred by patients who switch treatments is driven primarily by higher pharmacy costs.
“Our findings suggest that switching ART in stable patients only when there is clear clinical need may help curtail unnecessary expense—a critical consideration as the lifetime costs of HIV treatment continue to rise with the aging of the HIV-positive population,” the researchers concluded.
New drug regimens have improved outcomes for people with HIV making this once fatal illness into one that is chronic for many. Key to improvements in therapy has been the reduction in the number of pills needed for daily use as seen in the newest once-daily, single-tablet regimens.
Given the high price of these regimens, issues remain about the best way to administer them in a cost-effective way. Data indicate that second- and third-line treatment incur a greater cost. For patients who are stable on initial therapy, switching to a different regimen is more costly.










