Evolution of Care Within the Ambulatory Surgery Center
As the overall cost of care continues to rise, ambulatory surgery centers have transformed the healthcare landscape as a high-quality, low-cost alternative for many surgical procedures. Patient preference and the need to decrease healthcare costs are continuing to fuel the movement of services from hospital-based outpatient departments (HBODs) to freestanding ambulatory surgery centers (ASCs). This trend was largely made possible over the last several years by significant innovations in minimally invasive surgical procedures using laparoscopy and robotics, along with advances in anesthesia techniques, which reduce complications and recovery time.1 In the case of cardiac catheterization and percutaneous coronary intervention (PCI), the technological advancement in closure devices and the move to radial access have made the procedures faster and safer.2 Based on outcomes across the country, the outpatient setting for many types of surgery has proven to be both effective and safe, while also saving hospitals money.
While there is limited information on trials performed specifically within an ASC, there are several trials, such as the Radial Same-Day Discharge after PCI trial, which showed similar outcomes with no significant clinical differences, and no differences in procedural complications (3.7% vs 2.5%, P=.43, re-hospitalization (4.1% vs 4.1%, P=.92), re-intervention (2.5% vs 2.1%, P=.77), myocardial infarction (0% vs 0%, P=1.0) and all-cause mortality (0% vs 0%, P=1.0).3 Barnes Jewish Hospital took it a step farther in their February 2018 study “Novel Patient-Centered Approach to Facilitate Same-Day Discharge (SDD) in Patients Undergoing Elective Percutaneous Coronary Intervention.”4 Amin et al were able to increase the number of patients eligible for same-day discharge to 75% of patients undergoing elective PCI despite patient complexity. Of 230 patients with SDD, only 16 would have qualified under the Society for Cardiovascular Angiography and Interventions (SCAI) expert consensus guidelines developed in 2009. However, by using Amin et al’s patient-centered approach to selecting patients, the number eligible was significantly increased and adverse outcomes were not statistically different between the same-day discharge and the non-same-day discharge groups.
Patients enjoy both the convenience of the ASC setting and the out-of-pocket cost savings when utilizing an ASC. ASCs are typically able to streamline the registration, and both the admission and discharge processes, which shrinks the overall amount of time the patient spends at the facility on the day of the procedure. The convenience seems to far surpass that of hospital registration and pre-surgical processes.

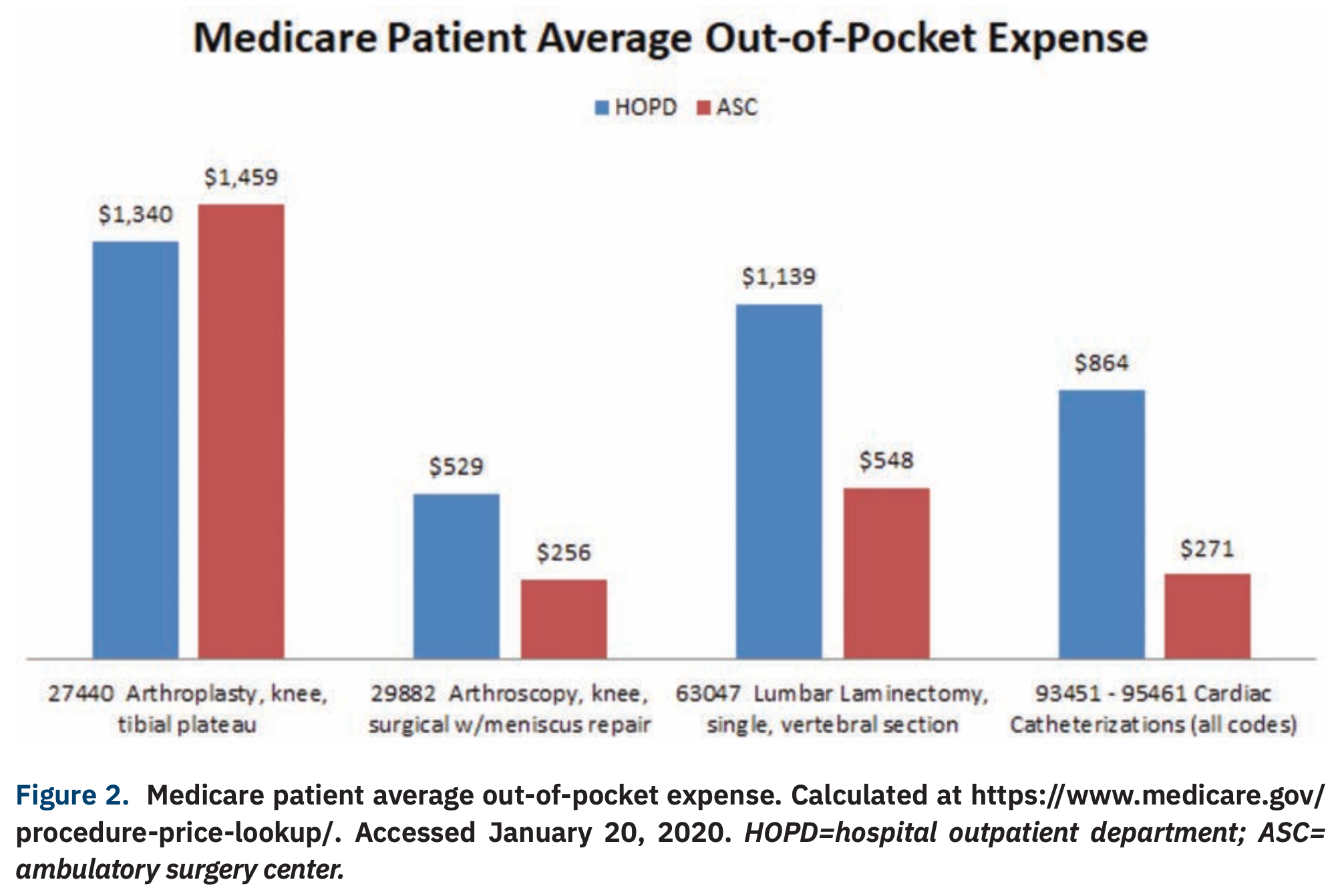
Financially, the difference can be quite large. For example, BlueCross/BlueShield in 2016 showed an out-of-pocket savings of $320 for lumbar/spine surgery and a savings of $1062 for outpatient angioplasty when done in an ASC.5 Medicare typically reimburses ASCs at a lower rate than it reimburses HOPDs for the same procedure and this often results in less out-of-pocket expense for Medicare patients (Figures 1-2).
With quality and safety being equal, insurers, including CMS, favor procedures being completed in the lower-cost ASC setting. With significant out-of-pocket cost savings for the patient, surgery in this setting is gaining popularity. As a result, not only is the overall number of ASCs increasing, but the financial market share is growing even faster. From 2016 to 2017, ASCs increased by 2.4%, whereas in prior years, 2012 to 2016, ASCs grew at only 1% per year.6 The ASC financial market is predicted to grow by 265% between 2017 and 2024, growing from $25.5B to $93.0B.7

Corazon believes that ASCs are where most care is headed. In fact, planning for procedural moves into an outpatient setting was involved in nearly every client engagement of ours over the past year. Cardiology overall is now seeing a shift to ASCs. Corazon has seen a large migration of cardiac catheterization procedures to the ASC after CMS’s 2019 addition of 12 separately payable diagnostic cardiac catheterization procedures to the ASC covered procedures list.8 Those numbers will continue to rise with the CMS addition of 6 cardiac interventional procedures to the approved list in 2020.9 CMS is also not the only payer moving in this direction. In some states with proper licensure and payer agreements, private insurers like United Healthcare, Cigna, and Humana are already covering coronary stenting in the ASC setting.
Also occurring across the country are some innovative partnerships between cardiovascular physicians and companies like National Cardiovascular Partners or ACA Cardiovascular in states like Florida, California, Arizona, Kansas, Louisiana, and Texas, where hybrid office-based labs (OBLs)/ASCs are prevalent. These centers often alternate between days functioning as an ASC and days functioning as an OBL in order to allow maximization of reimbursement based on site of service. Many states, however, do not allow for hybrid OBL/ASCs, and even if they are permitted, there can be significant hurdles in the Certificate of Need (CON) process. These centers also face challenges with recruitment of new independent surgeons and cardiovascular providers. In 2007, 70% of cardiology practices were independent and only 8% were hospital owned. Those numbers have now reversed, with 73% now being hospital-employed as of 2018.10
Can a hospital with employed cardiologists afford to see volume pulled away to a freestanding competitor? With cardiology being one of the most profitable hospital service lines, hospital administrators need to analyze the effect this out-migration of volume will have on the bottom line and strategically plan the next move. Does it make sense to build an ASC? Should a hospital partner with physicians in an ASC joint venture? Or should hospitals partner with existing ASC owners? Should a hospital create a Center of Excellence to support the higher hospital outpatient department reimbursement? These are all critical questions to consider in the coming year and beyond. This shift is already well underway in many areas across the country, and individual markets can be more or less affected.
There are both challenges and opportunities to be evaluated in the decision-making process. A detailed market analysis and feasibility study should be completed to ensure a facility or program is not “overbuilt” without the volume to support it. Understanding how to design a center to maximize space and efficiency, without paying rent for unnecessary space, or sinking capital in land and space, is critical. A strong business plan to validate the right service lines in the ASC will maximize revenue and optimize the staffing model. It will also be important to solidly negotiate contracts with payors and supply vendors.
While all of these challenges need to be addressed, the opportunities can be a big win for an organization. The opportunity to increase market share is possible through recapturing surgical volumes that have migrated to an outside ASC and/or by drawing in new patient volumes as people increasingly choose less-invasive surgery that is provided in a setting significantly more convenient than a hospital. Often it is easier for an ASC partnered with (or owned by) a hospital to recruit surgeons. The profit margin can be high in ASCs due to the narrow range of services provided, which allows for not only more efficient operation than the hospital OR, but also greater flexibility in staffing.
Competition in the ASC market is quickly expanding as for-profit companies and private equity firms jump in to capture this potential windfall. Many hospitals are caught between giving up the extra revenue from HOPDs and the risk of losing market share to lower revenue ASCs. Corazon believes it is critical that hospitals balance the short-term goal of maintaining higher revenues and the long-term goals of maintaining/increasing market share. This can be achieved by developing strategies and establishing the appropriate timing of shifting cases to the ASC setting. Without such strategies, hospitals stand the risk of missing out on this inevitable trend.
Corazon offers strategic program development for the heart, vascular, neuroscience, and orthopedic specialties. Corazon has a full continuum of consulting, accreditation, software solution, recruitment, and interim management services for hospitals, health systems and practices of all sizes across the country and in Canada. To learn more, visit www.corazoninc.com or call (412) 364-8200. To reach the co-author, email mluffey@corazoninc.com.
- A report by the Deloitte Center for Health Solutions. Growth in outpatient care – The role of quality and value incentives. Deloitte Insights. August 15, 2018. Available online at https://www2.deloitte.com/us/en/insights/industry/health-care/outpatient-hospital-services-medicare-incentives-value-quality.html?icid=dcom_promo_featured%7Cus;en#endnote-sup-1. Accessed January 20, 2020.
- Toth M. 6 reasons CMS should cover PCI in the ambulatory setting. Cath Lab Digest 2019 July; 26(7): 34. Available online at https://www.cathlabdigest.com/content/6-reasons-cms-should-cover-pci-ambulatory-setting. Accessed January 20, 2020.
- Rodriguez-Araujo G, Cilingiroglu M, Mego D, et al. Same versus next day discharge after elective transradial PCI: The RAdial SAme Day DischArge after PCI trial. (The RASADDA-PCI trial). Cardiovasc Revasc Med. 2018 Sep; 19(6S): 7-11. doi: 10.1016/j.carrev.2018.05.020.
- Amin AP, Crimmins-Reda P, Miller S, et al. Novel patient-centered approach to facilitate same-day discharge in patients undergoing elective percutaneous coronary intervention. J Am Heart Assoc. 2018 Feb 15;7(4). pii: e005733. doi: 10.1161/JAHA.117.005733.
- Blue Cross Blue Shield. How consumers are saving with the shift to outpatient care. The rise of “shoppable” surgical interventions. Available online at https://www.bcbs.com/the-health-of-america/reports/how-consumers-are-saving-the-shift-outpatient-care. Accessed January 20, 2020.
- MedPAC. Report to the Congress: Medicare Payment Policy. Ambulatory surgical center services (Ch. 5). March 2017. Available online at http://www.medpac.gov/docs/default-source/reports/mar17_medpac_ch5.pdf?sfvrsn=0. Accessed January 20, 2020.
- Bass J. Advisory Board Cardiovascular Roundtable – Cardiovascular Ambulatory Strategy. Webconference Recording. Available online to subscribers at https://www.advisory.com/research/cardiovascular-roundtable/events/webconferences/2019/cardiovascular-ambulatory-strategy/ondemand. Accessed January 20, 2020.
- January 2019 Update of the Ambulatory Surgical Center (ASC) Payment System. Available online at https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNMattersArticles/downloads/MM11108.pdf. Accessed January 20, 2020.
- Medicare Program: Changes to Hospital Outpatient Prospective Payment and Ambulatory Surgical Center Payment Systems and Quality Reporting Programs. A Rule by the Centers for Medicare & Medicaid Services. Federal Register. November 21, 2019. Available online at https://www.federalregister.gov/documents/2018/11/21/2018-24243/medicare-program-changes-to-hospital-outpatient-prospective-payment-and-ambulatory-surgical-center. Accessed January 20, 2020.
- Chacko R. Private practice today For early career cardiologists. American College of Cardiology. January 21, 2019. Available online at https://www.acc.org/membership/sections-and-councils/early-career-section/section-updates/2019/01/21/11/57/private-practice-today-for-early-career-cardiologists. Accessed January 20, 2020.