What is the Life Expectancy for Your Lead Apron? Are Your Lab Teams Protected?
Introduction
Every year and especially at the beginning of the academic year, we have requests from new cath lab staff and some faculty or fellows about getting a new lead apron for procedures using fluoroscopy. As an owner of an old lead apron, I was asked, “How long do our old lead aprons last?” The answer, of course, is “that depends.” How many times is it used every day? Is it folded, dropped, put on a hanger? There are other factors, but from a quick review (on the internet) it seems that lead aprons should last about 10 years. Defects (cracks, tears) are assumed to appear, on average, at about 5 years. In some labs, the fabrics or stitching has torn or frayed, and requires replacement. My current lead apron is one such example (Figure 1). In 2015, we talked about checking the lead aprons and other radiation protection methods.1 I thought it would be a good time to review the subject and update our cath lab practices.

Variables Impacting Lead Protective Qualities
A number of factors impact the life of an x-ray apron. These include the frequency of daily use, the manner in which it is stored (hung up) and the handling of the lead during donning and doffing. X-ray aprons should never be folded. Cracks in the lead lining can develop at the fold, reducing the useful life of the apron (Figure 2). Properly caring for your lead apron is essential to getting the most useful life from your apron.

Lead Apron Integrity Inspection
It is recommended to have the lead apron examined fluoroscopically at least once a year. The x-ray apron should be inspected annually or per manufacturer recommendations. The process is straightforward and often done in conjunction with the hospital’s radiation safety officer. The fluoroscopic inspection starts with placing the apron on the x-ray table. Then scan and examine the entire x-ray apron using the fluoroscope. The results of the inspection should follow your facility’s or state’s radiation safety protocols.
Lead aprons are required protection for anyone working in or around areas with ionizing radiation (cath and electrophysiology labs, fluoroscopic areas in the operating room, pulmonary or intensive care unit, or emergency department). Any individual risking exposure to radiation must wear protective garments. Lead aprons or skirt/vest combination garments should have sufficient shielding. Lead aprons absorb 90-95% of scattered radiation that reaches them. Lead aprons generally have shielding equivalence equal to an 0.25-0.5 mm lead and thus do not completely block, but only attenuate, the radiation. A lead apron with an 0.35 mm lead thickness equivalence should be sufficient for most fluoroscopic procedures. For high workloads, a wrap-around lead apron with an 0.25 mm lead equivalence that overlaps on the front, and provides 0.25+0.25=0.5 mm lead equivalence on the front and 0.25 mm on the back would be ideal. For a low workload, an 0.25 mm lead equivalence apron should do well.
Lead aprons protect sensitive body organs and also reduce the total body effective exposure dose by up to 85%. Wrap-around lead aprons are useful when medical personnel face away from the tube and away from the patient. Logically, then, when using aprons which are not 360-degree coverage, operators and staff should not turn away from the tube during beam activation.
In addition to the body lead apron (shoulder to mid-calf), a neck or thyroid lead collar is standard. The thyroid is very radiosensitive and hence, the lead collar protects the thyroid from the minimal exposure, reducing the total effective dose by a factor between 1.7 and 3. For eye protection to reduce the change of cataracts, some personnel wear protective 0.15 mm lead-equivalent glasses or goggles that limit the eye lens dose and provide about 70% attenuation even in high energy (kVp) beams. Protective eyeglasses reduce eye exposure during fluoroscopy. Leaded eyewear is recommended for personnel with high exposure, such as those who accumulate monthly radiation badge readings >400 mrem (4 Sv). Levels of exposure in this range are typically encountered only in areas where continuous cineangiography is performed (e.g., the cardiac catheterization laboratory).
Where Should I Stand During a Fluoroscopic Procedure?
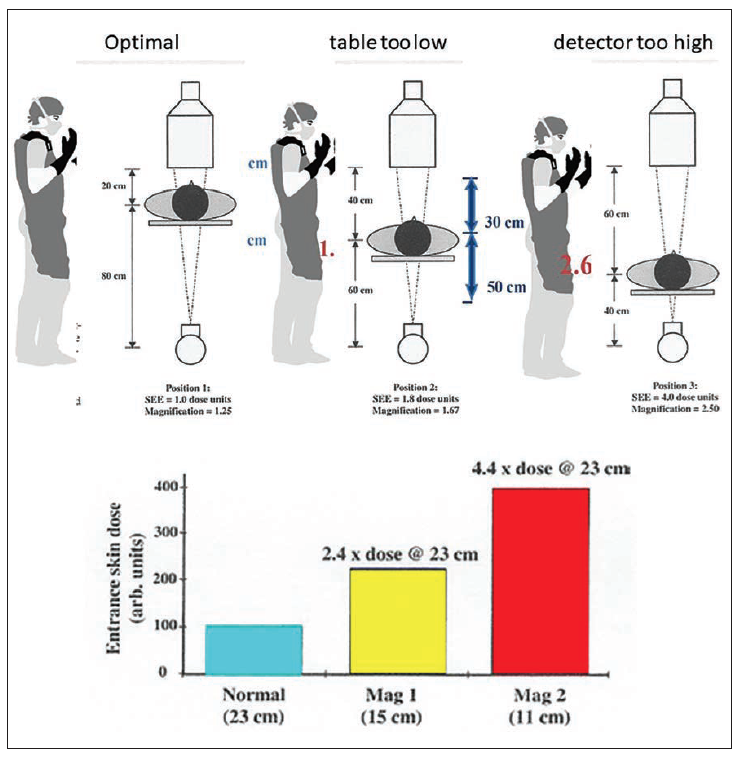
Radiation scatter and exposure at a distance depends on the angle of the gantry and distance of the x-ray tube to the patient (Figure 3). The tube position relative to the patient and the table height (Figure 4) will determine the amount of radiation scatter. Oblique views increase exposure dose, with the high dose coming from lateral views. Higher image intensifier distance from the patient also increases radiation scatter.


The operator should be aware of these controllable variables, and take an active role in protecting the staff by holding back on fluoro when someone steps close to give medications or forgets to move the portable shield into position. Real-time fluoro dose monitor badges are useful in order to display the exposure each individual receives during the case on a screen near the monitors (Figure 5) (see the study by Murat et al in this month’s issue for more information on real-time dosimetry).

Measurements have shown that scattered radiation from a patient’s body is more intense at the entrance side of x-ray beam, i.e., on the side where the x-ray tube is located. Therefore, it is better to stand on the side of the detector — that is, the exit side — and not on the x-ray tube side during a fluoroscopic procedure (Figure 6). Typically, only around 1% to 5% of the radiation to the patient’s body comes out on the exit side. Standing on the side of transmitted beam, scattered radiation corresponds to only 1% to 5% of the incident beam intensity. One the opposite side, radiation corresponding to 100% of the entrance beam intensity may occur.

The Bottom Line
The life of lead aprons discussion leads our thinking on ways to keep up best practices for safety and the best place to work. Table 1 summarizes routine methods to limit radiation exposure. As a group working in a radiation environment, it is everyone’s obligation to remain aware of reducing both personal and lab exposure.


References
1. Kern M, et al. Your lead is cracked? Radiation safety revisited. Cath Lab Digest. 2015 Nov; 23(11). Accessed June 24, 2021. Available online at https://www.hmpgloballearningnetwork.com/site/cathlab/article/Your-Lead-Cracked-Radiation-Safety-Revisited
Suggested Reading
Science Direct. Lead Apron. Accessed June 24, 2021. Available online at https://www.sciencedirect.com/topics/medicine-and-dentistry/lead-apron
International Atomic Energy Agency (IAEA). Radiation protection of medical staff in interventional procedures. Accessed June 24, 2021. Available online at https://www.iaea.org/resources/rpop/health-professionals/interventional-procedures/radiation-protection-of-medical-staff-in-interventional-fluoroscopy
Roguin A, Nolan J. Radiation protection in the cardiac catheterisation lab: best practice. Heart. 2021 Jan; 107(1): 76-82.
Hirshfeld JW Jr, Ferrari VA, Bengel FM, et al. 2018 ACC/HRS/NASCI/SCAI/SCCT Expert Consensus Document on optimal use of ionizing radiation in cardiovascular imaging: best practices for safety and effectiveness: a report of the American College of Cardiology Task Force on Expert Consensus Decision Pathways. J Am Coll Cardiol. 2018 Jun 19; 71(24): e283-e351.











