Intravascular Optical Coherence Tomography for the Diagnosis and Treatment of Peripheral Arterial Disease
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of Cath Lab Digest or HMP Global, their employees, and affiliates.
Mehmet Cilingiroglu, MD, FSCAI, FACC, FESC, FAHA1; Thomas Milner, PhD2; Ibrahim Halil Inanc, MD, FSCAI, FACC, FESC3; Deniz Mutlu, MD4; Kostas Marmagkiolis, MD, FSCAI, FACC5; Cezar Iliescu, MD, FSCAI, FACC6
1Professor of Medicine, Surgery and Biomedical Engineering; Mehmet Cilingiroglu, MD, Inc., San Diego, California; 2Professor of Biomedical Engineering and Surgery, Director, Michael E. DeBakey Center for Nano-Biophotonics, Baylor College of Medicine, Houston, Texas; 3Associate Professor of Cardiology, Phoenixville Hospital, Phoenixville, Pennsylvania; 4Cardiologist, Center for Coronary Artery Disease, Minneapolis Heart Institute Foundation, Minneapolis, Minnesota; 5Adjunct Associate Professor of Medicine, MD Anderson Cancer Center, Houston, Texas; 6Professor of Medicine, Director of Cardiac Catheterization Laboratories, MD Anderson Cancer Center, Houston, Texas

Disclosures: The authors report no conflicts of interest regarding the content herein.
Contact Mehmet Cilingiroglu, MD, at cilingiroglumehmet@gmail.com

Peripheral arterial disease (PAD) and chronic limb-threatening ischemia (CLTI) remain the leading cause of limb loss in the United States. Recently, the Society of Cardiovascular Angiography and Interventions (SCAI) was involved in the publication of a multisociety, multidisciplinary document for the clinical use of intravascular ultrasound (IVUS) in PAD and deep venous interventions.1 Although this document outlined the clinical use of intravascular imaging in PAD and CLTI patients, it did not include use of intravascular optical coherence tomography (OCT) for the diagnosis and treatment of these patients. Our group has extensive experience in the use of OCT in our daily clinical practice for PAD and CLTI cases as both a diagnostic and therapeutic tool.2-6 We present a case series below.

Case 1: Endovascular Revascularization of a Long Superficial Femoral Artery Chronic Total Occlusion
A 58-year-old female with a history of hypertension, hyperlipidemia, and tobacco use presented with Rutherford class III right lower-extremity claudication and an abnormal ankle-brachial index (ABI) of 0.5 despite maximal medical therapy and supervised graded exercise program. She was referred for direct peripheral angiography and possible intervention. Her peripheral angiography showed a long chronic total occlusion (CTO) of the right superficial femoral artery (SFA) extending from its ostium to the mid-distal segment, reconstituting in the adductor canal via collaterals (Figure 1A-C). A 6 French (Fr) crossover sheath was placed in the left common femoral artery and an .035-inch angled Glidewire (Terumo Interventional Systems) was advanced into the right SFA ostium. After dissection with subintimal tracking and reentry into the distal true lumen, the Glidewire was advanced to the right popliteal artery. It was then exchanged for an .014-inch guidewire and frequency domain (FD) OCT (C7-XR; Abbott) of the SFA was performed by injecting dextran to clear the blood. OCT imaging demonstrated long dissection planes with false and true lumens (Figure 2A-C). After confirming that the guidewire was in the true lumen, balloon angioplasty was performed using a 5.0 mm x 200 mm balloon, and the lesion was stented with a 5.0 mm x 220 mm Supera stent (Abbott) and post dilated with a 6.0 mm x 200 mm balloon (Figures 1D-F). Repeat OCT after stent deployment showed optimal stent expansion and wall apposition (Figures 2D-F). The patient was placed on dual antiplatelet therapy with significant clinical improvement and normalization of her ABI at 30-day follow-up.

Case 2: OCT-Guided Atherectomy and Drug-Coated Balloon for SFA Lesions
A 62-year-old female with history of hypertension, hyperlipidemia, diabetes, and known PAD was referred for management of lifestyle-limiting claudication of her right lower extremity despite maximal medical therapy. Her right lower-extremity ABI was 0.7, and she was referred for invasive peripheral angiography and possible intervention. A peripheral angiogram showed focal sequential lesions in her right SFA (Figure 3A). Using right groin access, a 6 Fr crossover sheath was placed. An .014-inch guidewire was advanced into the popliteal artery and OCT imaging was performed at baseline (Figure 4A-C). Measurements were made to delineate an accurate reference vessel diameter (Figure 4B-C) as well as minimal luminal diameter (Figure 4A) at the lesion sites. A fibrocalcific plaque was well described at the lesion site (Figure 4A). We performed OCT-guided directional atherectomy of the focal lesions using a Pantheris device (Avinger) (Figure 5A-B), followed by balloon angioplasty with a 6.0 mm x 80 mm drug-coated balloon with good results (Figure 3B-E). Repeat OCT imaging showed plaque removal without any dissection, clot, or residual significant stenosis (Figures 4D and 4F). The patient was treated with dual antiplatelet therapy for 1 month with significant improvement in her symptoms during follow-up.

Case 3: Orbital Atherectomy and OCT-Guided Percutaneous Transluminal Angioplasty for Popliteal CTO

A 67-year-old gentleman with right lower extremity lifestyle-limiting claudication and abnormal ABI was referred to our institution for a right leg arterial angiogram and possible endovascular intervention. A 5 Fr sheath was placed in the left common femoral artery. A 5 Fr tennis racquet catheter was used for the abdominal aortogram and a 5 Fr internal

mammary (IM) catheter for the selective right femoral angiogram after left-to-right crossover. A chronic, subtotally occluded right distal popliteal stenosis extending to the tibioperoneal trunk was identified and we elected to go ahead with a endovascular recanalization approach. The 5 Fr sheath was exchanged for a 6 Fr, 45 cm long sheath. A 300 cm, .014-inch Regalia guidewire (Asahi Intecc) was advanced to the right posterior tibial artery and a baseline OCT was performed (Figure 6). Due to significant calcification identified with OCT, we decided to perform an
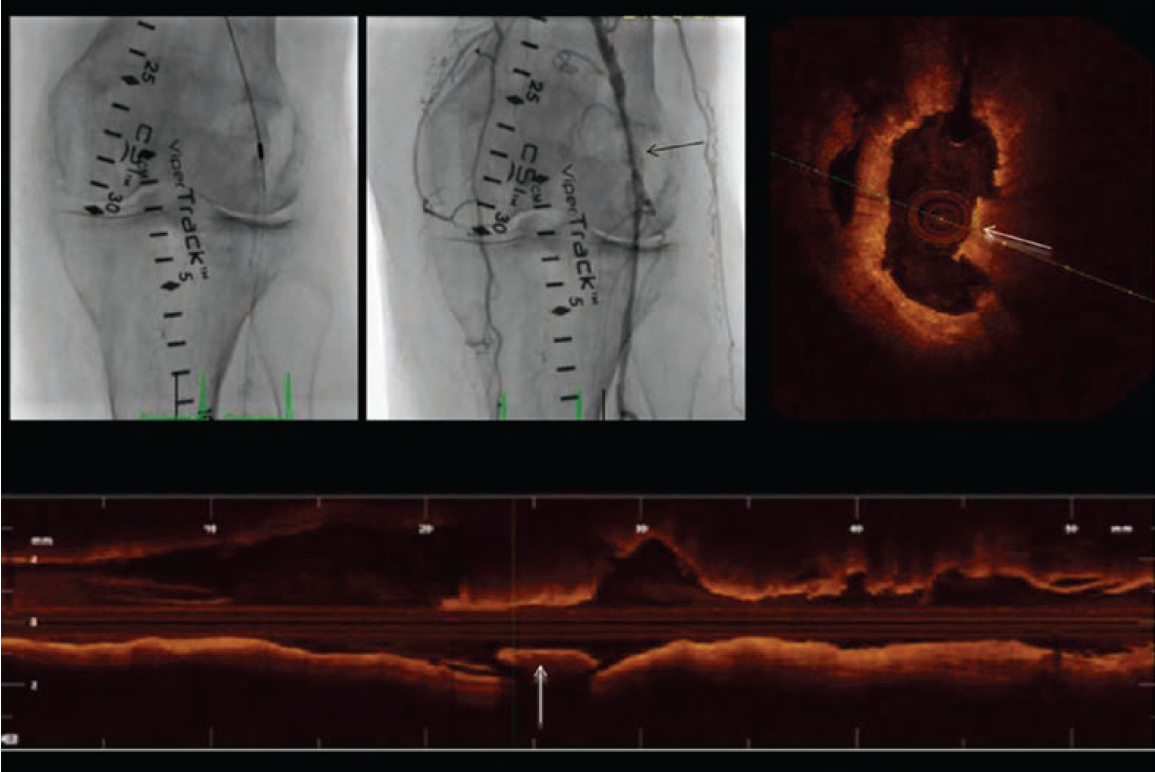
orbital atherectomy recanalization using the Diamondback 360 atherectomy device (Cardiovascular Systems, Inc.) in the affected segment. Although atherectomy established excellent angiographic flow, due to mild angiographic “haziness” at the site of intervention, we elected to perform a follow-up OCT (Figure 7). OCT demonstrated multiple segments of endothelial protrusion in the arterial lumen. Although data regarding the clinical significance of such OCT findings is currently absent, we decided to proceed with a 3.5 mm × 100 mm × 150 mm Sterling balloon (Boston Scientific) angioplasty. Final angiographic and OCT imaging showed good results (Figure 8).

angioplasty, with a good final result.
Final Thoughts
We have been using OCT for our PAD and CLTI patients for the following indications:
1) Understanding of the specific lesion characteristics (calcified, fibrotic, etc.);
2) Reference vessel dimension and lesion length;
3) Preventing geographic miss based purely on peripheral angiography;
4) Image-guided plaque removal in a more controlled fashion;
5) Visualizing specific device treatment effects on vascular healing.2-6
Even though FDA approval for the clinical use of OCT for PAD and CLTI has not yet occurred, we believe that the time has arrived for the application of OCT in the diagnosis and treatment of this patient population.
References
1. Secemsky EA, Aronow HD, Kwolek CJ, et al. Intravascular ultrasound use in peripheral arterial and deep venous interventions: multidisciplinary expert opinion from SCAI/AVF/AVLS/SIR/SVM/SVS. J Soc Cardiovasc Angiogr Interv. 2024 Jan 9; 3(1): 101205. doi:10.1016/j.jscai.2023.101205
2. Cilingiroglu M, Kilic ID, Hoyt T, Baruah V, Milner T, McElroy A, Lendel V, Paixao A, Cawich I, Ramirez-Kelly L, Marmagkiolis K, Iliescu C, Feldman MD. DIAMondback Atherectomy With OCT Visualization for Calcified PAD Lesions (DIAMOCT-PAD Study). J Invasive Cardiol. 2022 Feb; 34(2): E117-E123. doi:10.25270/jic/21.00145
3. Marmagkiolis K, Lendel V, Cilingiroglu M. OCT evaluation of directional atherectomy compared to balloon angioplasty. Cardiovasc Revasc Med. 2015 Sep;16(6):373-5. doi:10.1016/j.carrev.2015.02.003.
4. Marmagkiolis K, Lendel V, Cawich I, et al. Optical coherence tomography to guide below-the-knee endovascular interventions. Int J Cardiol. 2014 Oct 20; 176(3): 1336-1338. doi:10.1016/j.ijcard.2014.07.145
5. Cawich I, Paixao AR, Marmagkiolis K, Lendel V, Rodriguez-Araujo G, Rollefson WA, Mego DM, Cilingiroglu M. Immediate and intermediate-term results of optical coherence tomography guided atherectomy in the treatment of peripheral arterial disease: Initial results from the VISION trial. Cardiovasc Revasc Med. 2016 Oct-Nov; 17(7): 463-467. doi:10.1016/j.carrev.2016.07.002
6. Inanc IH, Mutlu D, Marmagkiolis K, Iliescu C, Ates I, Feldman M, Cilingiroglu M. CRT-400.18 Use of IVOCT for assessment of the lesion characteristics as well as evaluation of vascular healing effects of different technologies in PAD patients. J Am Coll Cardiol Intv. 2023 Feb, 16 (4_Supplement) S64. https://www.jacc.org/doi/10.1016/j.jcin.2023.01.207










