4 Cases: Treating Uncontrolled Hypertension With the Paradise™ Ultrasound Renal Denervation System (uRDN)
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of Cath Lab Digest or HMP Global, their employees, and affiliates.
Surabhi Madhwal Atreja, MD, FACC, RPVI;
Aravinda Nanjundappa, MBBS, MD;
Wissam Gharib, MD, FACC, FSCAI, and Jordan King, MPAS, PA-C;
Vamsee Yaganti, MD, MA, FACC, FSCAI
Renal denervation has emerged as a promising adjunctive therapy for patients on three or more blood pressure medications who continue to experience resistant hypertension. The Paradise™ Ultrasound Renal Denervation (uRDN) System (Recor Medical) uses ultrasound-based ablation, delivering circumferential energy to the renal arteries and targeting sympathetic nerves with controlled precision while helping to preserve the endothelium.
As renal denervation continues to gain clinical traction, interventional cardiologists and advanced practice providers play a key role in integrating this technology into hypertension management strategies. Here, clinicians describe four patients experiencing uncontrolled hypertension, their treatment with uRDN, and the resulting blood pressure reduction for each patient.
 Case #1: uRDN in an 82-Year-Old Female With Uncontrolled Hypertension
Case #1: uRDN in an 82-Year-Old Female With Uncontrolled Hypertension
Surabhi Madhwal Atreja, MD, FACC, RPVI
Health Sciences Clinical Professor; Director, Hypertension Clinic; Certified Hypertension Specialist UC Davis Health, Sacramento, California
Patient History. An 82-year-old female with a past medical history of hypertension, arthritis, rheumatoid arthritis, hypothyroidism, migraine, and remote seizures was referred for evaluation of uncontrolled hypertension. Despite maximal medical therapy, including amlodipine 10 mg, lisinopril 40 mg, a combination diuretic (triamterene and hydrochlorothiazide), spironolactone, and a beta blocker (labetalol), her blood pressure (BP) remained persistently elevated, measuring 200/80 mmHg across multiple visits to her primary care provider. Given her refractory hypertension, her primary care physician referred her to the Resistant Hypertension Clinic, a multidisciplinary team including cardiology, nephrology, and endocrinology.
Ambulatory blood pressure monitoring demonstrated an average BP of 160/75 mmHg at home, ranging up to 194 mmHg systolic, despite adherence to lifestyle and medical therapy. She attempted to optimize medication timing, taking most of her doses in the morning due to persistently elevated readings. Given her high cardiovascular risk, with a 50% increased likelihood of a major cardiac event over four years, further evaluation was warranted.
Workup for secondary hypertension was unremarkable, including normal TSH, renin-aldosterone ratio, and catecholamines. Her estimated glomerular filtration rate (eGFR) was 58. Renal artery ultrasound and computed tomography (CT) imaging for procedural planning confirmed patent renal arteries without stenosis and no adrenal pathology. Echocardiography revealed concentric hypertrophy and diastolic dysfunction, consistent with longstanding hypertension. At this stage, the only remaining pharmacologic option was clonidine, which would introduce a seventh medication. Given her poor blood pressure control, high cardiovascular risk, and medication burden, she was considered a suitable candidate for renal denervation, despite her age. The patient, after experiencing years of struggling with severe hypertension, agreed to proceed.

Procedure. The patient underwent renal denervation (RDN) using the Paradise Ultrasound Renal Denervation System under conscious sedation.
• Access and Angiography: A 5 French Omni Flush catheter (Angiodynamics) was introduced via femoral access over an .035-inch J-tipped wire, and an aortogram confirmed patent bilateral renal arteries without stenosis.
• Renal Anatomy Assessment: The right renal artery exhibited early bifurcation, while the left renal artery was long.
• Selective Angiography: Using a mother-and-child technique, a 5 French internal mammary (IM) diagnostic catheter was inserted via a 7 French renal double curve (RDC) guide, allowing for selective renal artery intubation. The renal artery was then selectively wired with an .014-inch Spartacore wire (Abbott). The 5 French IM catheter was removed. A selective angiogram was done, and quantitative angiography was used to assess renal artery size.
• Ultrasound-Based Renal Denervation:
o Right renal artery: Due to an early bifurcation, two ablation spots were applied with 4.2 mm catheter, with approximately 7 seconds of ablation for each denervation.
o Left renal artery: A 5 mm catheter and three non-overlapping ablation spots were successfully delivered, with approximately 7 seconds of denervation for each.
A final renal angiogram confirmed vessel integrity, with no evidence of dissection, thrombosis, or complications.

Result. The patient remained hemodynamically stable post procedure but exhibited a rapid and significant reduction in blood pressure.
• Immediate Response: Her blood pressure dropped markedly, prompting overnight observation instead of standard same-day discharge. Initial concerns that the drop was due to sedation were dismissed after sustained reductions over 24 hours.
• Follow-Up at Five Months:
o Blood pressure: 144/67 mmHg (previously 200/80 mmHg)
o Medication reduction:
- Labetalol 300 mg BID was maintained;
- Lisinopril was reduced to 20 mg PRN;
- Three antihypertensive agents were discontinued.
Given her dramatic BP reduction (~55 mmHg systolic), further medication reduction was not pursued as she experienced symptomatic hypotension when her BP dropped below 140 mmHg. The patient has been discharged from the specialty resistant hypertension clinic and continues follow-up with her primary care physician.
 Case #2: uRDN in a 77-Year-Old Female With Resistant Hypertension Over Two Decades
Case #2: uRDN in a 77-Year-Old Female With Resistant Hypertension Over Two Decades
Aravinda Nanjundappa, MBBS, MD Department of Cardiovascular Medicine, Cleveland Clinic, Cleveland, Ohio
Patient History. A 77-year-old female with a 20-year history of resistant hypertension was referred for further evaluation. Resistant hypertension is defined by persistent above-goal BP despite use of three antihypertensive drug classes including a long-acting calcium channel blocker, a renin angiotensin blocker, and a diuretic. Over the years, multiple antihypertensive regimens had been attempted, but the patient experienced intolerance to high-dose diuretics due to hypokalemia. Despite optimized medical therapy and a 24-hour ambulatory blood pressure monitor confirming an average BP >140/80 mmHg, her office BP on the day of the procedure remained at 150/90 mmHg.

The patient had already incorporated lifestyle modifications, including a low-salt diet, increased fruit intake, and regular exercise (10-15 minutes of walking, 2-3 times per week), but BP control remained inadequate. Although she had previously experienced hypertensive urgency requiring emergency department visits, no recent episodes had occurred within the past year. An extensive secondary hypertension workup, including renal artery duplex ultrasound and aldosterone levels, was unremarkable. She was referred for renal denervation and consented to the procedure.
Procedure. Renal denervation was performed using the Paradise Ultrasound Renal Denervation System via a percutaneous femoral approach.
• Vascular Access: Right femoral artery access was obtained at an optimal location to minimize vascular complications. A 5 French sheath was initially placed.
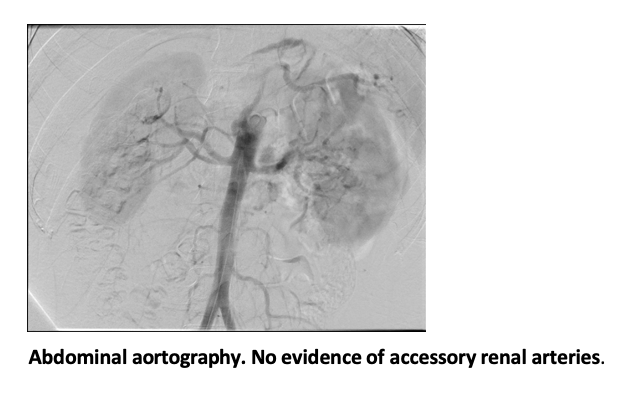
• Renal Artery Imaging: A 5 French pigtail catheter was used for nonselective aortography, confirming single renal arteries bilaterally with a bifurcation on the right side. No significant abnormalities were noted in the renal parenchyma.
• Selective Renal Angiography: The sheath was upgraded to a 7 French Brite Tip sheath (Cordis), and a 7 French Mach 1 guide catheter*(Boston Scientific) was introduced using a no-touch technique to minimize trauma to the aorta. An .035-inch guidewire was placed across the aorta, followed by an .014-inch support wire (Spartacore, Abbott) to selectively wire the renal arteries.
• The right renal artery measured 5 mm and left renal artery measured 5.2 mm.
The Paradise Ultrasound RDN catheter was used for ultrasound-based ablation of renal artery sympathetic nerves.

Right Renal Artery Treatment:
• Due to the distal renal artery bifurcation, the main renal artery renal denervation was planned for 2 treatments, each balloon spaced 5 mm apart.
• The balloon was positioned and inflated. Complete vessel wall contact was determined by evaluating the cessation of any flow across the balloon before delivering ultrasound energy.
• The patient received conscious sedation to manage mild discomfort during denervation pulses.
• Nitroglycerin was administered post ablation to prevent vasospasm.
• Final angiography confirmed intact renal perfusion without evidence of dissection, perforation, spasm, or stenosis.
Left Renal Artery Treatment:
• The left renal artery was shorter in length, requiring careful positioning of the denervation catheter to avoid branch points and ostial segments.
• The balloon was adjusted proximally to achieve complete wall apposition before energy delivery.
• Similar to the right side, two denervation applications were performed at 5 mm spacing.
• Final angiography confirmed normal renal perfusion and no procedural complications.
Throughout the procedure, heparin (50-60 U/kg) was administered to prevent thrombotic complications. There were no vascular complications, and renal function remained stable post procedure. Aspirin (81 mg) was prescribed as the only post-procedural therapy, and no additional antiplatelets were required.

Result. At six-week follow-up, 24-hour ambulatory BP monitoring demonstrated an 8-10 mmHg reduction in systolic BP, with an average BP of 135-136/84 mmHg. The patient remained on her existing antihypertensive regimen, with plans to reassess medication adjustments at six months. At this early postprocedural stage, no antihypertensive agents were discontinued; however, as renal denervation effects continue to evolve over 3-6 months, future medication de-escalation will be considered, depending on sustained BP response at six months.
Acknowledgements. Thank you to Drs. Amar Krishnaswamy, Navneet Sharma, and Deepak Gajanana, and the Cardiac Catheterization Laboratory Staff at Cleveland Clinic for their support.
Case #3: uRDN in a Younger Male With Severe Hypertension and Multiple Emergency Admissions
Wissam Gharib, MD, FACC, FSCAI, and Jordan King, MPAS, PA-C Mon Health, Morgantown, West Virginia
 Patient History. A 54-year-old male with a history of severe, difficult-to-control hypertension was referred for further evaluation. Despite being on three to four antihypertensive medications, his blood pressure remained consistently high, often exceeding 200 mmHg systolic. His medication regimen required frequent adjustments due to intolerances, particularly orthostatic symptoms that prevented adherence to certain medications.
Patient History. A 54-year-old male with a history of severe, difficult-to-control hypertension was referred for further evaluation. Despite being on three to four antihypertensive medications, his blood pressure remained consistently high, often exceeding 200 mmHg systolic. His medication regimen required frequent adjustments due to intolerances, particularly orthostatic symptoms that prevented adherence to certain medications.
Before his initial evaluation, he had five emergency department visits, and two hospital admissions for hypertensive urgency. He had been diagnosed with a transient ischemic attack (TIA) during one of his admissions for hypertensive urgency. The persistently high blood pressure was affecting his quality of life.
His body mass index (BMI) was 31 kg/m² and he had a history of diabetes, but his hypertension was suspected to have a strong genetic component, given a family history of severe, difficult-to-control hypertension and coronary artery disease. Given his recurrent hospital visits, medication intolerance, and persistent hypertensive crises, renal denervation (RDN) was considered a reasonable adjunct therapy.
Procedure. The patient underwent renal denervation during his hospital admission using the Paradise Ultrasound RDN System via a percutaneous femoral approach. Right femoral artery access was obtained. Renal artery imaging confirmed no significant stenosis or abnormalities. Three ablations were performed in the right and left renal arteries. Final angiography confirmed vessel integrity with no evidence of complications. The procedure was well tolerated, and the patient was discharged the same day with no immediate changes to his medication regimen.
Results. At one-month follow-up, his blood pressure had significantly improved, ranging between 110-140 mmHg systolic, compared to consistently exceeding 200 mmHg pre-procedure.
Patients with chronic severe hypertension often experience a period of adjustment as their bodies adapt to lower BP levels. However, this patient reported feeling significantly better, without the fatigue or sluggishness that some patients experience as their BP normalizes. At three months post procedure, he continued to do well and he was beginning to wean off anti-hypertensive medication. His BP remained in a healthy range and his day-to-day quality of life had improved dramatically.
Conclusion and the Role of the Advanced Practice Provider. This case illustrates the importance of renal denervation as an adjunctive therapy for patients with severe, medication-intolerant hypertension.
• Renal denervation provided significant blood pressure reduction (this patient saw a ~60 mmHg–90 mmHg drop in systolic BP, an unexpected, unusual, and dramatic reduction in BP that is far greater than what has occurred in our other patients thus far or in the clinical trials).
• The patient avoided additional emergency visits or hospitalizations post procedure.
The role of the advanced practice provider (APP) is critical for early intervention and post-procedural follow-up, as well as for identifying candidates for renal denervation, monitoring response, and ensuring patient education. In this case, the APP played a vital role in the initial evaluation and referral for renal denervation, as well as post-procedure follow-up. APPs can help monitor BP stability and symptomatic improvement, and provide patient counseling on expectations, medication adherence, and long-term BP monitoring.
This patient’s early response suggests that renal denervation may offer a life-changing benefit in select younger patients with genetically driven, treatment-resistant hypertension. Ongoing follow-up at six months and one year will further assess durability and potential medication reductions.
 Case #4: uRDN in a 77-Year-Old Male With Severe Uncontrolled Hypertension and Multiple Comorbidities
Case #4: uRDN in a 77-Year-Old Male With Severe Uncontrolled Hypertension and Multiple Comorbidities
Vamsee Yaganti, MD, MA, FACC, FSCAI Director, Structural Heart Disease; Interventional Cardiologist, St. Mark’s Hospital, Salt Lake City, Utah
Patient History. This is a 77-year-old male with a history of longstanding hypertension who presented for evaluation of persistently uncontrolled blood pressure despite maximal medical therapy. He had a complex cardiovascular history, including:
• Chronic systolic heart failure, New York Heart Association (NYHA) class 2 (initially 43%, improved to 65% in 2024);
• Coronary artery disease status post PCI of the obtuse marginal 2 artery in 2015 and left anterior descending (LAD) in December 2016;
• Type 2 diabetes mellitus;
• Severe pulmonary hypertension;
• Moderate mitral regurgitation;
• Moderate aortic insufficiency;
• Paroxysmal atrial fibrillation with CHA2DS2-VASc score 6;
• Ascending aortic aneurysm;
• History of gastrointestinal bleeding;
• History of pulmonary embolism/deep vein thrombosis;
• Obstructive sleep apnea on CPAP.
His hypertension had been poorly controlled for nearly a decade, with prior hospital admissions in 2016 and 2017 for CHF exacerbation secondary to noncompliance with antihypertensive medications and diuretics. After being lost to follow-up for seven years, he was seen again in 2024 with acute on chronic systolic heart failure in the setting of hypertensive urgency. This time, however, the patient demonstrated good medication adherence but continued to have persistently elevated BP (178/115 mmHg on presentation).
His antihypertensive regimen consisted of five medications (amlodipine, carvedilol, hydralazine, isosorbide mononitrate, losartan)at different times of the day, yet his blood pressure remained difficult to control. Given his high cardiovascular risk and history of heart failure exacerbations, renal denervation was considered as an adjunct to his pharmacologic regimen. The patient was counseled that the primary goal of RDN was blood pressure control in conjunction with medications, rather than complete medication withdrawal. It was additionally emphasized to the patient that he continue to pursue lifestyle modifications that include sodium restriction and weight loss.
His pre-procedure workup included:
• CT angiography to assess renal artery anatomy (confirming suitability for RDN);
• Laboratory testing to rule out secondary hypertension (renin, aldosterone, TSH);
• Extensive lifestyle counseling, emphasizing sodium restriction (≤1.5g/day), weight loss, and dietary modifications;
• BMI assessment (37.6 kg/m²).
After completion of his preprocedure workup, he was considered to be an ideal candidate for renal denervation.

Procedure. RDN was performed in November 2024, using the Paradise Ultrasound RDN System via a right femoral approach.
• Vascular Access and Imaging:
o Right common femoral artery access was obtained.
o A diagnostic angiogram confirmed patency of bilateral renal arteries without >30% stenosis.

• uRDN Treatment:
o Right renal artery: An 8 mm balloon was selected. Three ultrasound ablation applications were performed in the main renal artery, avoiding small branches.
o Left renal artery: An 8 mm balloon was selected. Three ultrasound ablation applications were performed in the main renal artery, avoiding small branches.
o Final angiography confirmed angiographically normal renal arteries with no evidence of dissection, thrombosis, or spasm.
• Post-Procedure Care and Discharge: The groin access site was closed using a Perclose device (Abbott), facilitating early ambulation (within 2 hours). The patient was discharged home the same day with standard postprocedural instructions to avoid lifting >10 lbs for five days, monitor for groin hematoma, and continue his antihypertensive regimen without immediate changes.
Outcomes. At one-month follow-up:
• Office BP: 125/74 mmHg (compared to 178/115 mmHg pre-procedure)
• Home BP monitoring: Stable between 120-130 mmHg systolic
• Medication adjustment: Hydralazine reduced from 50 mg TID to 25 mg TID due to lower BP and mild fatigue
• Overall BP reduction: ~50 mmHg systolic, ~40 mmHg diastolic
The patient remains asymptomatic with no complications from the procedure. In the interim and at six-month follow-up, further medication adjustments are planned if BP control remains stable. Importantly, clinical trial data (eg, RADIANCE™ studies) suggest sustained BP reduction for at least three years post RDN. To assess durability and long-term efficacy, patients are followed at one month, six months, and one year.
This article is sponsored by Recor Medical, Inc.
Jordan King, MPAS, PA-C, and Drs. Atreja, Nanjundappa, Gharib, and Yaganti are a paid consultants of Recor Medical, Inc., and have been compensated for their time and expertise in participating in this content.
Paradise is a registered trademark and RADIANCE is a trademark of Recor Medical, Inc.
Find More:
Cardiovascular Ambulatory Surgery Centers (ASCs) Topic Center
The Latest Clinical & Industry News
Grand Rounds With Morton Kern, MD
Peripheral Artery Disease Topic Center










