A Selection of News From the Transcatheter Cardiovascular Therapeutics (TCT) Meeting, October 22-26, 2012, Miami, Florida
Analysis of Medtronic Stent Finds Early Cessation of Dual Antiplatelet Therapy Caused No Increased Risk of Blood Clots to One Year
More than 900 patients in RESOLUTE clinical program interrupted or discontinued DAPT after 30 days following implant procedure
 Interrupting dual antiplatelet therapy after 30 days following the implantation of a Resolute drug-eluting stent from Medtronic, Inc. caused no increase in rates of stent thrombosis at one year, according to a new analysis of the global RESOLUTE clinical program presented October 23rd at the 24th Annual Transcatheter Cardiovascular Therapeutics (TCT) scientific symposium, and presented by Prof. Sigmund Silber, MD, director of the Heart Centre at the Isar in Munich, Germany.
Interrupting dual antiplatelet therapy after 30 days following the implantation of a Resolute drug-eluting stent from Medtronic, Inc. caused no increase in rates of stent thrombosis at one year, according to a new analysis of the global RESOLUTE clinical program presented October 23rd at the 24th Annual Transcatheter Cardiovascular Therapeutics (TCT) scientific symposium, and presented by Prof. Sigmund Silber, MD, director of the Heart Centre at the Isar in Munich, Germany.
The global RESOLUTE clinical program consisted of a large, randomized, controlled trial and a series of confirmatory single-arm studies involving nearly 250 sites in 32 countries across Europe, Asia, the Pacific Rim, the Middle East, Africa, Latin America and North America. In total, the program enrolled 5,130 patients who received a Resolute drug-eluting stent.
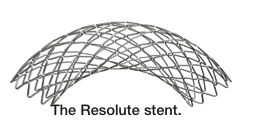 The new analysis of dual antiplatelet therapy interruption included data on nearly 5,000 patients for whom the relevant information was available and used the Academic Research Consortium (ARC) definitions of stent thrombosis.
The new analysis of dual antiplatelet therapy interruption included data on nearly 5,000 patients for whom the relevant information was available and used the Academic Research Consortium (ARC) definitions of stent thrombosis.
The analysis examined the one-year rates of stent thrombosis in patients whose dual antiplatelet therapy was interrupted after one month and three months following their implant procedure.
- 907 patients interrupted or discontinued their dual antiplatelet therapy after one month. None of these patients (0.0 percent) experienced ARC definite/probable stent thrombosis through one year of follow-up.
- 816 patients interrupted or discontinued their dual antiplatelet therapy after three months. Similarly, none of these patients (0.0 percent) experienced ARC definite/probable stent thrombosis through one year of follow-up.
Prior Cardiac Surgery Does Not Mean Worse Outcomes for STEMI Patients Who Receive Stents
 Contrary to previous data, patients with prior open heart surgery, or coronary artery bypass graft surgery (CABG), who have a ST-elevation myocardial infarction (STEMI) and receive a coronary stent have similar outcomes to patients without previous CABG, based on study of a large, prospective, regional STEMI network, being presented Oct. 23 at the 2012 Transcatheter Cardiovascular Therapeutics (TCT) conference.
Contrary to previous data, patients with prior open heart surgery, or coronary artery bypass graft surgery (CABG), who have a ST-elevation myocardial infarction (STEMI) and receive a coronary stent have similar outcomes to patients without previous CABG, based on study of a large, prospective, regional STEMI network, being presented Oct. 23 at the 2012 Transcatheter Cardiovascular Therapeutics (TCT) conference.
Recognizing that the majority of data indicating worse outcomes for STEMI patients with prior CABG came from an older era of heart attack treatment, researchers at the Minneapolis Heart Institute Foundation and Minneapolis Heart Institute® (MHI) at Abbott Northwestern Hospital in Minneapolis sought to assess contemporary outcomes in its regional STEMI network from April 2003 to December 2011.
“Traditionally, it is believed that patients with prior CABG are at much higher risk, are less likely to receive reperfusion therapy and have worse outcomes; thus, these patients have been frequently excluded from clinical trials,” explains Timothy D. Henry, MD, an interventional cardiologist at the MHI at Abbott Northwestern and director of research with the Minneapolis Heart Institute Foundation. “As a result, there is limited contemporary data on these challenging patients, and they often didn’t receive the current standard of care for STEMI, which is percutaneous coronary intervention (PCI).”
Of the 3,552 consecutive STEMI patients in the study, 7.1 percent had prior CABG. These patients were older, more frequently male and had increased prevalence of diabetes. The prior-CABG group also had lower baseline ejection fraction, lower current smoking rates and were less likely to have a lesion identified as the clear culprit of the heart attack.
“In addition, these patients frequently have abnormal baseline EKGs and challenging coronary anatomy,” Dr. Henry said. “While patients with prior-CABG in this study did have a slightly lower rate of reperfusion, our reperfusion rate was still much higher compared with previous studies.”
Patients in both groups had similar door-to-balloon times and both in-hospital stays (4.8 vs. 5 percent) and 30-day stays (4.8 vs. 5.7 percent) were similar. At one year, patients with prior CABG had a numerically higher mortality (10.8 vs. 9 percent) that was not statistically significant.
Prior studies have suggested increased mortality in patients with prior CABG, but that “may have reflected the lower rates of reperfusion and older PCI strategies,” according to the study authors.
“The outcomes of both arms are excellent and very similar, which is promising,” Dr. Henry states. “The one group in whom the outcomes were slightly worse — but not statistically worse — were those prior-CABG patients in whom the saphenous vein graft was the culprit lesion for the heart attack.”
Based on their findings, the researchers concluded that STEMI outcomes in patients with prior CABG, regardless of the culprit lesion, may be as good as STEMI patients overall when treated with a uniform protocol with the same rapid treatment.
“These results are another example of the benefits of a regional STEMI network, and its ability to provide more unified care,” Henry stated.
Cappella Medical Announces Long Term Follow-Up Results for Its Sideguard® Side Branch Coronary Stent at TCT 2012
 Cappella Medical Devices Ltd, a medical device company developing solutions for the treatment of coronary bifurcation disease, announced the multicenter, long-term follow-up results for its Sideguard® coronary side branch stent. Long-term follow-up data on the Sideguard stent was obtained from 399 patients from the United Kingdom, Germany, and Italy. The MACE rate was: 3.7% (30 day F/U), 7.1% (6 mo F/U) and 10.2% (1 year F/U) comparing favorably with existing standard practice.
Cappella Medical Devices Ltd, a medical device company developing solutions for the treatment of coronary bifurcation disease, announced the multicenter, long-term follow-up results for its Sideguard® coronary side branch stent. Long-term follow-up data on the Sideguard stent was obtained from 399 patients from the United Kingdom, Germany, and Italy. The MACE rate was: 3.7% (30 day F/U), 7.1% (6 mo F/U) and 10.2% (1 year F/U) comparing favorably with existing standard practice.
These data represent the largest multicenter clinical experience to date with the Sideguard technology. The Sideguard was developed to protect the ostium of the side branch in the treatment of bifurcation disease. Results from this multicenter experience have confirmed that preservation of the side branch of diseased coronary arteries by protecting the ostium has clear, long-term benefits when compared to existing standard practice of provisional and two-stent procedures.
Dr. Farzin Fath-Ordoubadi, Consultant Cardiologist and Cath Lab Director at the Heart Centre, Manchester Royal Infirmary, commented, “The Sideguard stent can be used to treat complex bifurcation lesions in a straightforward manner, with excellent clinical outcomes. The long term follow up data from this multicenter study validate the fact that a dedicated bifurcation technology that protects the ostium of the side branch is a viable alternative to the more traditional provisional and two-stent strategies when treating coronary side branch disease.”
Up to 30% of all PCI patients have bifurcation disease, yet there has not been one proven dedicated treatment. Treating these patients has always been a challenge for physicians due to the complex anatomy of the coronary side branch. Gary Brogan, VP of Regulatory and Clinical Affairs at Cappella, stated, “The provisional and two-stent techniques used today all involve manipulating the straight DES stent struts in an attempt to provide clear access into the side branch. Data is now being presented documenting the negative flow dynamic and shear stress issues of floating stent struts. We are confident that these positive results are due to the Sideguard platform that scaffolds the ostium, reducing plaque and carina shift while preserving the side branch.”
The Sideguard delivery system features a proprietary split-sheath, balloon-released technology that ensures precise placement on the ostial borderline. The Sideguard self-expanding nitinol stent promotes continuous wall apposition and positive remodeling and its unique trumpet-shaped design conforms to varying characteristics of the side branch ostium.
The Cappella Sideguard system is currently CE-mark approved and is being distributed throughout Europe, South America, India, and Canada. Cappella Medical Devices Ltd., Galway, Ireland is the R&D and manufacturing subsidiary of Cappella, Inc. For more information, please visit www.cappella-med.com.
SUPERB Trial and SUPERA 500 Registry Both Demonstrate Highest Reported Patency Rates and Zero Fracture Rates for IDEV Supera Peripheral Stent
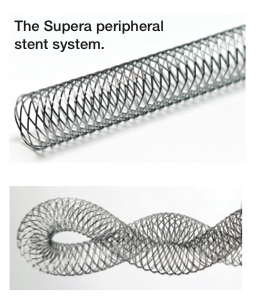 IDEV Technologies, Inc. (IDEV) announced the presentation of consistent positive clinical outcomes of the Supera® Peripheral Stent System from its SUPERB pivotal U.S. clinical trial and SUPERA 500 long-term registry conducted in Germany. IDEV’s data confirms clinical evidence for Supera’s highly differentiated, disruptive and proprietary stent design. The presentation at the 24th Annual Transcatheter Cardiovascular Therapeutics (TCT) scientific symposium was given by co-primary investigator Lawrence Garcia, MD, Chief, Interventional Cardiology and Vascular Interventions at Steward St. Elizabeth’s Medical Center.
IDEV Technologies, Inc. (IDEV) announced the presentation of consistent positive clinical outcomes of the Supera® Peripheral Stent System from its SUPERB pivotal U.S. clinical trial and SUPERA 500 long-term registry conducted in Germany. IDEV’s data confirms clinical evidence for Supera’s highly differentiated, disruptive and proprietary stent design. The presentation at the 24th Annual Transcatheter Cardiovascular Therapeutics (TCT) scientific symposium was given by co-primary investigator Lawrence Garcia, MD, Chief, Interventional Cardiology and Vascular Interventions at Steward St. Elizabeth’s Medical Center.
SUPERB, a Food and Drug Administration (FDA) Investigational Device Exemption (IDE) trial, demonstrated the highest patency rates in peripheral IDE stent trials for superficial femoral or proximal popliteal artery disease that have been publically reported (86% based on survival analysis at 12 months). In addition, it is the first femoral-popliteal artery IDE trial to record zero stent fractures for bare or drug coated nitinol-based technologies.
The SUPERA 500 Registry included a highly challenging real-world patient population of 495 patients, 750 stents, and a mean stent length of nearly 13 cm, with 45% and 41% of the Supera stents placed in the distal SFA and proximal popliteal artery, respectively. The one and two-year patency rates were 84.1% and 73%, respectively, as measured by duplex ultrasound. Consistent with the SUPERB trial, there were zero reported stent fractures at one year and also at two years in the SUPERA 500 registry.
The Supera stent’s interwoven nitinol wire technology platform offers significantly improved radial strength, flexibility and kink resistance, and is designed to adapt to the motion of the vascular anatomy. The SFA and popliteal arteries are exposed to significant mechanical stress with bending and rotation of the knee, and represent a harsh environment for any endovascular device. An ideal stent for use in these areas should offer range of motion without interrupting the anatomical function of the arteries.
Data from the SUPERB trial will be utilized for IDEV’s premarket approval (PMA) application with the FDA, which the Company anticipates filing in the fourth quarter of 2012.
The SUPERB Trial (Comparison of the SUPERA PERipheral System to a Performance Goal Derived from Balloon Angioplasty Clinical Trials in the Superficial Femoral Artery) is an FDA-approved IDE trial to evaluate Supera in treating patients with obstructive SFA and proximal popliteal artery disease.
SUPERB data analysis was performed independently and validated by the Harvard Clinical Research Institute (HCRI).
The Supera stent is currently indicated in the United States for the palliative treatment of biliary strictures produced by malignant neoplasms and in multiple other countries for the treatment of biliary strictures produced by malignant neoplasms and for peripheral vascular use following failed percutaneous transluminal angioplasty (PTA).
For more information, please visit www.idevmd.com.
Simple, Inexpensive Risk Score Can Shorten Length of Stay for MI Patients
 One day can lead to an estimated savings of nearly $7,000 in total hospital costs
One day can lead to an estimated savings of nearly $7,000 in total hospital costs
A simple-to-use risk score can identify low-risk patients following a non-ST elevation myocardial infarction (STEMI) and may provide an opportunity to employ early discharge strategies to reduce length of hospital stay and save hospital costs without compromising the safety of the patient, based on a study presented by the Minneapolis Heart Institute Foundation on Oct. 23 at the 2012 Transcatheter Cardiovascular Therapeutics (TCT) conference.
Recently, there has been an emphasis on lowering both hospital length of stay and hospital readmission in patients with STEMI, to decrease costs to the overall healthcare system. STEMI patients in the U.S. have lower length of stay in the hospital but increased rates of hospital readmissions compared with other countries.
The Zwolle PCI Risk Index Scoring System is validated to identify low-risk STEMI patients for early discharge. “This is a simple-to-calculate risk score, which takes into account age, three-vessel disease, Killip Class, anterior infarction, ischemic time and TIMI flow post,” says the study’s senior author Timothy D. Henry, MD, an interventional cardiologist at the Minneapolis Heart Institute® (MHI) at Abbott Northwestern Hospital and director of research with the Minneapolis Heart Institute Foundation. “These risk factors can be easily and quickly assessed by the healthcare professionals within a hospital.”
For the study, Craig E. Strauss, MD, MPH, a cardiologist at MHI at Abbott Northwestern, and colleagues retrospectively applied the Zwolle Risk Score to all STEMI patients presenting to their large, regional STEMI system between January 2009 and December 2011.
Among the 967 cases, 44 percent were classified as high risk and 56 percent as low risk. High-risk patients were older, had more hypertension, diabetes and previous coronary artery disease, were more likely to have had previous revascularization and had lower left ventricular ejection fractions.
The low-risk patients had statistically significant lower mortality rates than the high-risk patients in the in-hospital setting (0 vs. 11.9 percent), at 30 days (0.2 vs. 12.9 percent) and at one year (3.9 vs. 16.4 percent). Likewise, the low-risk patients had fewer complication rates across the board: any complication (6.5 vs. 17.1 percent), heart failure (0.3 vs. 2.1 percent), cardiogenic shock (0.3 vs. 5.1 percent) or new dialysis (0 vs. 1.7 percent).
“Because there is increasing pressure to reduce rising hospital costs while also reducing readmissions, this study’s findings are particularly important,” says Dr. Henry. “We found that identifying low-risk patients in an easy, inexpensive manner can lead to safe discharge a full day in advance of the high-risk STEMI patients.”
The discharge of one day in advance for these low-risk patients led to a savings of nearly $7,000 in total hospital costs.
“Prospective use of this risk score may provide an opportunity to safely employ early discharge strategies to reduce length of stay and total hospital costs without compromising patient safety,” the study authors concluded.
“This study’s findings have immediately manifested into a change in our clinical practice. As part of our overall quality improvement program, we are going to use the Zwolle Risk Score to identify low-risk patients, and these patients will avoid the cardiac critical care unit and will have a plan to be discharged in 48 hours,” adds Dr. Henry. “This change in patient management is the result of the safety findings with this low-risk patient population in the study.”
8500+ Patient Trial Validates Association Between High Platelet Reactivity and 1-Year Cardiovascular Outcomes at TCT 2012
 Patients with high platelet reactivity had 2.5 times greater rate of stent thrombosis at 1 year
Patients with high platelet reactivity had 2.5 times greater rate of stent thrombosis at 1 year
Accumetrics, Inc., developer of the VerifyNow® System, a point-of-care system for measuring platelet reactivity to multiple antiplatelet agents, announced the presentation of the 1-year results from the Assessment of Dual AntiPlatelet Therapy with Drug-Eluting Stents (ADAPT-DES) registry at the 2012 Transcatheter Cardiovascular Therapeutics (TCT) meeting. Study findings indicate a significant association between platelet reactivity and 12-month stent thrombosis, myocardial infarction, and death. ADAPT-DES had previously demonstrated an approximately four times greater rate of stent thrombosis at 30 days in patients with high residual platelet reactivity, as measured by Accumetrics’ VerifyNow P2Y12 Test. This association continued through follow-up, as patients with high residual platelet reactivity demonstrated a 2.5 times greater rate of stent thrombosis at 1 year. The VerifyNow P2Y12 Test and VerifyNow PRUTest are used to measure a patient’s platelet reactivity and the antiplatelet effect of medications such as clopidogrel and prasugrel (Plavix® and Effient®).
“The 1-year results from the ADAPT-DES Registry, the largest platelet reactivity registry conducted to date, show an irrefutable association between high PRU values and thrombotic events,” said Gregg W. Stone, MD, Professor of Medicine, Columbia University, Director of Cardiovascular Research and Education, Center for Interventional Vascular Therapy, New York-Presbyterian Hospital / Columbia University Medical Center and Principal Investigator of ADAPT-DES. “Decoupling bleeding risk from the benefit of reducing ischemic events is critically important for more potent therapies to have a positive net clinical benefit. This is an area we anticipate further exploring with ADAPT-DES data, to determine whether an optimal therapeutic window for platelet inhibition with ADP antagonists can be identified.”
Much like the commonly used PT/INR, there has been great interest within the cardiology community to identify levels of platelet reactivity where the risk for both thrombotic events and bleeding are minimized. This concept of a therapeutic window has been postulated in previously published reports.1,2,3
“The results from ADAPT-DES validate the published results from the past decade of research in the arena of platelet reactivity testing,” said Matthew J. Price, MD, Director of the Cardiac Catheterization Laboratory at Scripps Clinic, La Jolla, CA. “Thrombosis is still one of the most catastrophic events we face in the cath lab, with data demonstrating that almost 90% of stent thrombosis cases experience a recurrent MI or cardiovascular death. With the availability of generic clopidogrel and newer more potent P2Y12 inhibitors, we can use this information to aid us in providing the most cost effective and clinically appropriate treatment strategy for our patients.”
References
- Campo G et al. J Am Coll Cardiol. 2011;57:2474-2483.
- Gurbel PA et al. Am Heart J. 2010;160:346-354.
- Sibbing D et al. J Thromb Haemost. 2010;8:250-256.
Micell Technologies Announces Positive Data from Clinical Studies of MiStent Sirolimus-Eluting Absorbable Polymer Coronary Stent
Minimal progression of late lumen loss through 18 months; superior performance against primary endpoint
Micell Technologies, Inc. announced positive data from two clinical studies of its investigational MiStent® sirolimus-eluting absorbable polymer coronary stent system (MiStent SES™), a thin-strut drug-eluting stent distinguished by a rapid-absorbing drug/polymer coating designed to control drug release. Eighteen-month outcomes from the DESSOLVE I trial, and nine-month data supporting all study endpoints in the DESSOLVE II trial, were presented by David Kandzari, MD, Director of Interventional Cardiology and Chief Scientific Officer for the Piedmont Heart Institute of Atlanta, Ga. These data, presented at the 24th Annual Transcatheter Cardiovascular Therapeutics (TCT) scientific symposium held in Miami, Fla., will be available on the TCT website, www.tctmd.com, following the conference.
Dr. Kandzari said, “MiStent has demonstrated excellent results as well as treatment advantages we have not seen in other drug-eluting stents. Achieving minimal progression of late lumen loss from four- through 18-month assessments is unique and a significant positive clinical outcome. Once MiStent is available to physicians, this novel product will also present interventional cardiologists with a meaningful and important alternative in addressing the limitations of permanent polymer DES products. Indeed MiStent’s performance characteristics and clinical data can serve as a foundation for the improvement of patient care.”
Data presentations at TCT included the following:
1) Eighteen Month Clinical and Imaging Results from the DESSOLVE I First-in-Human Trial of the MiStent SES with Absorbable Polymer
The DESSOLVE I trial, the first clinical assessment of safety and efficacy of the investigational MiStent SES, treated thirty patients with de novo lesions in coronary arteries ranging in diameter from 2.5 to 3.5 mm and amenable to treatment with a maximum 23 mm length stent. Subjects were enrolled across five study centers in New Zealand, Australia and Belgium. Three independent subgroups of 10 patients each were evaluated using angiography, IVUS and OCT at three time points: four, six and eight months. The primary efficacy endpoint was in-stent late lumen loss. Safety was assessed by incidence of MACE and presence of strut coverage with tissue within the treated artery at each time point. William Wijns, MD, PhD, Cardiovascular Center, Aalst, Belgium and John Ormiston, MBChB, Mercy Angiography Unit, Auckland, New Zealand are co-principal investigators for this trial.
Results: MiStent SES mean in-stent late lumen loss (LLL) was essentially unchanged through 18 months post-procedure in patients with discrete de novo lesions in native coronary arteries. Initial angiographic evaluations on 25 subjects had a mean in-stent late lumen loss (LLL) of 0.07 mm. The mean 18-month LLL for the same 25 subjects was essentially unchanged at 0.09 mm. Intravascular ultrasound (IVUS) confirmed minimal change in neointimal hyperplasia in the long-term follow-up with an initial mean (± standard deviation) percent obstruction of 7.2±4.8% and 11.2±8.1% at 18 months. The major adverse cardiac events (MACE) rate at 18 months was unchanged from 12 months, with only one non-target vessel non-Q-wave myocardial infarction (MI).
2) Nine Month Imaging and Twelve Month Clinical Results from the DESSOLVE II Randomized Trial of the MiStent SES with Absorbable Polymer
The DESSOLVE II CE (Conformite Europeenne) Mark trial is a randomized, multi-center study of patients with documented stable or unstable angina pectoris. The primary endpoint is superiority of the MiStent SES in minimizing in-stent late lumen loss at nine months, compared to Medtronic’s Endeavor® Sprint DES, as measured by the angiography core laboratory in de novo coronary lesions in vessels ranging in diameter from 2.5 to 3.5 mm and amenable to treatment with a maximum 30 mm length stent. The DESSOLVE II study completed enrollment of 184 patients in July 2011. Data analysis confirms that DESSOLVE II met all study objectives, demonstrated a competitive in-stent late lumen loss, and achieved strong signal of safety. Micell has submitted these data as part of its application for a CE Mark.
MiStent SES demonstrated statistically superior performance as compared to the Endeavor® Sprint DES for the primary endpoint of in-stent LLL. At nine months’ follow-up, in-stent LLL was 0.27 mm with a target lesion revascularization (TLR) rate of 0.9%. The MACE rates were 4.3% for MiStent SES and 6.7% for Endeavor.
“DESSOLVE II, a randomized, controlled study, successfully met all endpoints. Patient evaluations at nine months confirmed that MiStent SES provided a healing profile comparable to that of a bare metal stent, with a median of only 0.3% uncovered stent struts, zero malapposition, and a return of normal endothelial function, with 100% of MiStent-treated vessels showing vasodilation. DESSOLVE II builds on the results of the first-in-human DESSOLVE I study, in which there was no increase in late lumen loss through 18 months post-procedure,” said Dennis J. Donohoe, MD, Micell’s Chief Medical Advisor.
The MiStent SES system includes a proprietary stent coating that contains crystalline drug (sirolimus) and an absorbable polymer. As the polymer softens and disperses from the stent into the adjacent tissue, the coating provides controlled and sustained release of therapeutic levels of drug within the surrounding tissue. These properties are intended to enhance safety as compared to conventional permanent polymer DES.
Results of animal studies have determined that the coating is cleared from the stent in 45 to 60 days, leaving a bare metal stent, and the polymer is completely absorbed into the surrounding tissue in 90 days to promote long-term patency and compatibility with the artery.
Using an approved drug (sirolimus) and polymer (PLGA), Micell’s patented supercritical fluid technology allows a rigorously controlled drug/polymer coating to be applied to a bare-metal stent. The MiStent SES uses Eurocor’s (CE Marked) Genius® Magic Cobalt Chromium Coronary Stent System, a bare-metal stent.
The MiStent Sirolimus Eluting Absorbable Polymer Coronary Stent System is an investigational device currently being evaluated in international clinical studies and is not yet approved or available for sale in any market.
Micell also is developing a drug-coated balloon for vascular interventions. Learn more www.micell.com.
Nitinol Stent Performs Better Than Balloon Angioplasty Alone in Treating Lesions of the Popliteal Artery
Results of the ETAP trial presented at TCT 2012
A study found that a nitinol stent performed better than balloon angioplasty alone in treating blockages of the popliteal artery, which runs through the leg behind the knee. Results of the ETAP trial were presented at the 24th annual Transcatheter Cardiovascular Therapeutics (TCT) scientific symposium.
Due to its location behind the mobile knee joint, it is controversial whether to implant a stent in the popliteal artery for all cases or only for cases in which balloon angioplasty alone results in a suboptimal result. In this study, investigators conducted a prospective, randomized, multi-center trial comparing primary nitinol stent placement to angioplasty alone in patients who had a single, de-novo obstructive lesion in the popliteal artery.
A total of 246 patients from nine centers in Europe were included in this trial. Patients were randomly assigned to either a self-expanding nitinol stent (N=119) or a standard balloon angioplasty procedure (N=127). The primary study endpoint was one-year duplex ultrasound-derived primary patency, defined as freedom from target lesion restenosis without further intervention. Secondary endpoints included target lesion revascularization, secondary patency, changes in Rutherford categories from baseline, and limb salvage rates. X-rays were taken at one year and examined for stent fractures.
The mean lesion length for the PTA group was 43.2 mm compared to 41.3 mm for the stent group. Six patients (2.4%) died during the follow up period. The one-year primary patency rate was significantly higher in the nitinol-stent group (67.4 percent) than in the balloon angioplasty group (44.9 percent, P<0.05). Post procedure target lesion revascularization rates were 15.4 percent for the stent group and 21.4 percent for the optimal angioplasty group (P=0.29). No significant differences between the treatment groups could be observed concerning secondary patency, limb salvage rates, and the clinical course by Rutherford categories. Two stent fractures were reported at one year.
Patients in the stent group also reported more improved walking distances at one year than the angioplasty group.
“Results from this trial indicate that treatment of popliteal artery obstructive lesions with a nitinol self-expanding stent is safe. Additionally, one-year primary patency and target lesion revascularization rates (including acute angioplasty failures) were substantially better with the nitinol stent than with balloon angioplasty,” said lead investigator Thomas Zeller, MD. Dr. Zeller is Professor of Clinic Cardiology and Angiology and the Chief of the Department of Angiology at Universitäts-Herzzentrum Freiburg Bad Krozingen in Germany.
The trial was supported by an unrestricted study grant by C.R. Bard. Dr. Zeller reported receiving consulting honoraria by C. R. Bard.
Study Confirms Benefits of Transcatheter Aortic Valve Replacement Over Three Years
Results of PARTNER Cohort B trial presented at TCT 2012
A study found that transcatheter aortic valve replacement (TAVR) yielded lower mortality rates after three years compared with medical therapy in patients deemed to be ineligible for conventional aortic valve surgery. Results of the PARTNER Cohort B trial were presented at the 24th annual Transcatheter Cardiovascular Therapeutics (TCT) scientific symposium.
TAVR is the recommended treatment for patients with severe aortic stenosis who are not suitable candidates for surgery. Outcomes beyond two years in such patients have not yet been extensively studied.
Inoperable patients with severe symptomatic aortic stenosis (AS) were randomly assigned to transfemoral TAVR or to standard therapy (which often included balloon aortic valvuloplasty) in the PARTNER trial. Data on three-year outcomes were analyzed according to intention to treat (ITT).
A total of 358 patients underwent randomization at 21 centers. The Kaplan Meier estimated rates of death at three years were 54.1 percent in the TAVR group and 80.9 percent in the standard-therapy group (P<0.0001); corresponding rates of cardiac death were 41.4 percent and 74.5 percent (P<0.0001). The survival advantage associated with TAVR that was initially observed at one year persisted during the subsequent years.
“After three years of follow-up, the benefits of TAVR were sustained as measured by all cause mortality, cardiovascular mortality, repeat hospitalization, and functional status,” said one of the investigators, E. Murat Tuzcu, MD. Dr. Tuzcu is Professor of Medicine and Vice-Chairman of the Department of Cardiology in the Sydell and Arnold Heart & Vascular Institute at the Cleveland Clinic.
“Three-year data continue to support the role of TAVR as the standard-of-care for symptomatic patients with aortic stenosis who are not surgical candidates,” said Dr. Tuzcu.
The trial was funded by Edwards Lifesciences. Dr. Tuzcu reported no financial conflicts of interest.










